Simple delivery method that enhances a promising cancer treatment
Posted: 11 April 2022 | Ria Kakkad (Drug Target Review) | No comments yet
Scientists have developed a delivery method that enhances treatment by adding CAR T cells and specialising signalling proteins to a hydrogel that is injected next to a tumour.
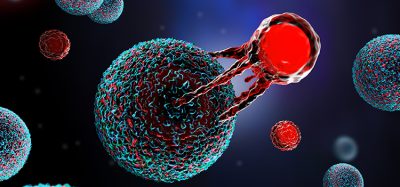
Scientists from Stanford University, US have developed a delivery method that enhances the “attack power” of the modified immune cells, CAR T cells. The researchers added CAR-T cells and specialised signalling proteins to a hydrogel and injected the substance next to a tumour. This gel provides a temporary environment inside the body where the immune cells multiply and activate in preparation to fight cancerous cells. The study, which was recently published in Science Advances, could pave way for a promising cancer treatment.
Currently, intravenous (IV) infusions are the main mode of administration for CAR-T cells. In this method, cells enter the bloodstream and flow through the entire body. But the approach is not ideal for treating solid tumours, which are often dense, exist in specific locations and have defences to hide from and fend off immune cells.
To activate CAR-T cells strongly enough to eradicate a tumour, the cells must undergo prolonged exposure to a high concentration of specialised signalling proteins. Called cytokines, these proteins tell the engineered immune cells to rapidly replicate and prepare to destroy the tumour. However, if delivered systemically through an IV drip, the number of cytokines required to launch an effective attack would be toxic to other parts of the body.
Instead, the researchers created a gel that can temporarily house cytokines and CAR-T cells near the tumour. The immune cells grow and proliferate there, inside the body, and are continuously released to bombard the cancerous growth.
The gel is made of water and two ingredients: a polymer made from cellulose, a material found in plants and biodegradable nanoparticles. When combined, the two components bind together but can easily be pried apart.
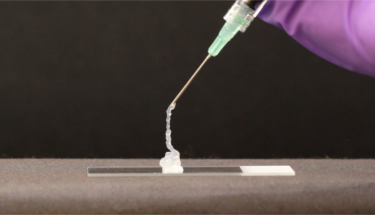
As shown in this demonstration, the hydrogel can be easily injected through a needle and then rapidly self-heals after injection to form a solid-like gel. The needle in this image is a 21-gauge needle, a relevant size for human injection
[Credit: Abigail K. Grosskopf].
The gel’s mesh-like configuration is woven tightly enough to prevent the tiny cytokines from slipping out. At the same time, the structure’s connections are weak enough for the CAR-T cells to break them and detach when ready to take down cancerous cells.
In mice, the researchers found that all experimental animals injected with gel containing both CAR-T cells and cytokines became cancer-free after 12 days. The team also tried delivering just CAR-T cells in the gel, but the tumours disappeared more slowly or not at all in some mice. Treatments delivered through an IV drip or in saline rather than in the gel were even less effective on the tumours. Additionally, the gel did not induce adverse inflammatory reactions in the mice, and it fully degraded within the body in a few weeks.
The team also tried injecting the gel treatment farther away from the tumour – on the opposite side of the mouse’s body from the cancerous growth. The animals’ tumours still vanished, although it took about twice as long as when treatment was added adjacent to the tumour.
NEWS: Discovery could advance CAR T-cell therapy
READ MORE
The researchers are now planning the next set of experiments which will further explore the gel delivery method’s ability to treat faraway tumours.
Related topics
Clinical Trials, Drug Delivery, Immuno-oncology, Immunotherapy, Oncology, Research & Development, Therapeutics
Related conditions
Cancer
Related organisations
Stanford University