A genetic approach to high insulin levels
Posted: 18 September 2017 | Dr Zara Kassam (Drug Target Review) | No comments yet
A team of researchers have succeeded in precisely describing the effects of a frequent genetic mutation in cases of congenital hyperinsulinism…

A team of researchers have succeeded in precisely describing the effects of a frequent genetic mutation in cases of congenital hyperinsulinism.
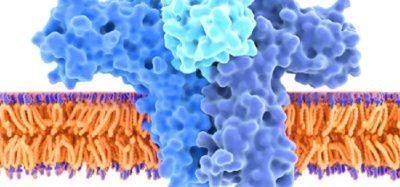
The researchers at the University of Geneva (UNIGE), Switzerland, supported by the Swiss National Science Foundation (SNSF) focused on a genetic mutation known to be associated with hyperinsulinism. This gene produces a protein known as GDH, which instructs the pancreas to release insulin. It normally behaves differently once the level of blood glucose passes a certain threshold.
Then GDH opens up to receive a molecule known as an accelerator that binds to it. In this way the protein moves into the active phase, which in turn sends a signal to the pancreas, causing it to produce more insulin.
This new study could pave the way for new treatments.
“We can imagine developing a drug that inhibits the GDH accelerator by occupying the same site, which would reduce the production of insulin,” said Lead Author Professor Pierre Maechler.
A drug of this type might also be used to treat obesity: if there is no insulin in the body, the person does not gain weight. The researchers point out that “The protein GDH could enable the production of insulin to be regulated. This type of approach, while appearing to offer an extremely simple solution, would, of course, raise questions and ethical problems. But we know that in some cases diets don’t work, and gastric bypass surgery is by no means a harmless solution either,” he added.
The team working with Prof Maechler are also studying the role of fructose in the development of type 2 diabetes. This discovery could confirm the suspected links between the massive use of fructose by the food industry since the 1980s and the sharp increase in the number of people with type 2 diabetes a few years later.
In congenital hyperinsulinism the mutant gene causes the structure of the protein to change. The protein remains permanently receptive to the accelerator molecule, whatever the level of glucose in the blood. As a result, it constantly sends signals to the pancreas, telling it to release insulin, which it then does excessively.
Insulin promotes the transfer of glucose to the muscles. If there is a constant surplus of insulin, it leads to undernourishment of the brain, which in turn results in brain damage and intellectual retardation, and to coma and even death in the most critical cases. Sugar is not the main culprit, though. “In these patients, even a meal consisting solely of protein will trigger the production of insulin,” Explains Prof Maechler.
The treatments currently available for congenital hyperinsulinism are problematic: they range from almost total removal of the pancreas, which produces diabetes artificially, to administration of drugs which regulate the activity of the pancreatic cells more or less precisely but have major side effects.
This discovery has been published in Human Molecular Genetics, could pave the way for new therapies.
Related topics
Drug Development, Proteomics, Research & Development
Related conditions
Diabetes
Related organisations
Swiss National Science Foundation, University of Geneva
Related people
Professor Pierre Maechler