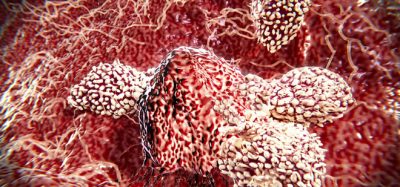
Cancer cells hide to evade immunotherapy
Posted: 24 September 2018 | Iqra Farooq (Drug Target Review) | No comments yet
Cancer cells have been found to evade immunotherapy by hiding behind human leukocyte antigens, with researchers identifying therapies to prevent relapse…
Researchers have identified that tumours can ‘hide’ from combination therapies, using a trio of genes – human leukocyte antigens.
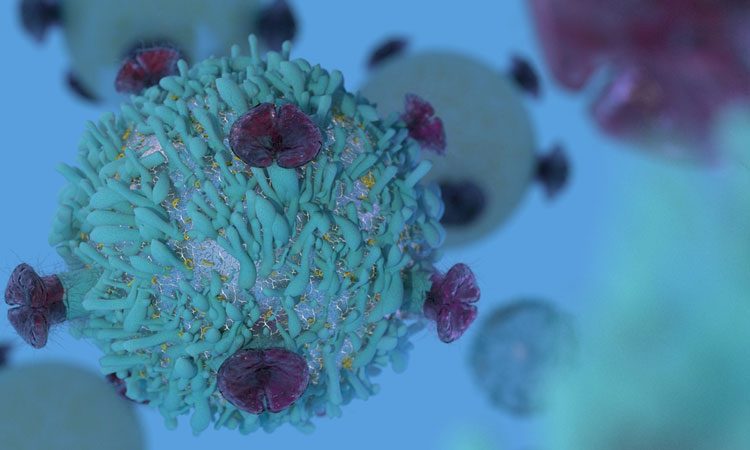
Using the immune system to treat cancer is promising for some patients, however for many, the response is short-lived.
Researchers from Fred Hutchinson Cancer Research Centre used a new technology to investigate how cancer cells change under the pressure of immunotherapy treatments. The newly developed method for measuring molecules in single cells deeply analyses the response of patients with Merkel cell carcinoma to a combination immunotherapy. Merkel cell carcinoma is a rare skin cancer caused by a common virus.
“Twenty percent of Merkel cell patients have an initial response to immunotherapy but then relapse – it’s been unclear why,” said first author, Dr Kelly Paulson, senior fellow at Fred Hutch. “Understanding the cause of relapse allows us to design immunotherapies that can get toward long-term tumor control to make cancer a more chronic disease.”
Dr Paulson and Dr Aude Chaupis studied cancer cells from two patients who initially responded to the combination therapy. This therapy combined a checkpoint inhibitor with a T-cell therapy, which was capable of killing the cancer cells. The T-cell therapy involved taking T cells from patients, growing and multiplying them in a laboratory and then injecting them back into the patient.
Initially, cancers in both patients shrank form the therapy.
“We saw in both patients that the cancers went almost completely away,” said Dr Paulson. “The cancers were shrinking, and when we took biopsies we saw that the T cells actually got into the cancers and helped mediate this regression. That was exciting and the patients were doing great.”
The authors report that one patient went from nearly being admitted into a hospice to going back to work, and the other the cancer seemed to return but only in an isolated spot, and is still being controlled. After two years, the first patient returned with something resembling a bug bite on his leg. After analysis, it was confirmed that it was metastatic Merkel cell cancer.
“It grew quickly, it was biopsied and shortly after it showed up in multiple places,” mentioned Dr Paulson.
The researchers could not identify why the cancers had returned, and collaborated with coauthors Dr Paul Nghiem of the University of Washington, and Fred Hutch’s Dr Jason Bielas and Dr Raphael Gottardo to take a closer look at the molecular changes in T cells, tumour cells and other cells in the tumour microenvironment. They used single-cell RNA sequencing and were able to see that the tumour was specifically ‘hiding’ from the T cells.
Dr Paulson wanted to identify if this could be fixed and cultured cells from one patients, and applied drugs used for other cancers to it. She said the results could show which combination of therapies should be used when people relapse from immunotherapy treatment.
“We didn’t know what was going on with these patients and how their cancer was able to come back. Now we are able to understand what’s going wrong, and that gives us a way to fix it. It’s very obvious we need a multi-pronged approach rather than just one dagger that the cancer can escape,” said Dr Chapius.
The report was published in Nature Communications.
Related topics
Disease Research, Drug Development, Drug Targets, Immunotherapy, Oncology, Research & Development, T cells, Therapeutics
Related conditions
Cancer
Related organisations
Fred Hutchinson Cancer Research Centre
Related people
Dr Aude Chaupis, Dr Jason Bielas, Dr Kelly Paulson, Dr Paul Nghiem, Dr Raphael Gottardo