Triple treatment keeps lung cancer from coming back
Posted: 4 June 2015 | Victoria White
Lung cancer often returns and the recurring cancer is often resistant to the chemotherapy and other drugs that originally drove it into remission…
Lung cancer is responsible for some 1.59 million deaths a year.
That figure is due, in part, to the fact that the cancer often returns and the recurring cancer is often resistant to the chemotherapy and other drugs that originally drove it into remission. According to new research by the Weizmann Institute‘s Professor Yosef Yarden, a new strategy involving a three-pronged approach might keep an aggressive form of lung cancer from returning.
The research, says Yarden, arose out of some puzzling results of clinical trials. One class of relatively common lung cancers, which carry a particular mutation in a receptor on the cell membrane, called EGFR, can be treated using a drug that keeps a growth signal from getting into the cell, thus preventing the deadly progression and spread of the cancer. But within a year, those with this mutation invariably experience new cancer growth, usually as a result of a second EGFR mutation.
To prevent this from happening, researchers had tried to administer another drug, an antibody that is today used to treat bowel cancer. This drug also obstructs the passing of the growth signal by stopping EGFR. Even though the antibody drug should have been able to effectively block the EGFRs, including those generated by the second mutation, clinical trials of this drug for lung cancer did not produce results. “This finding ran counter to everything we knew about the way tumours develop resistance,” says Yarden.
How do the cancer cells manage to circumvent the blockade put up by an anti-EGFR antibody? In a new study, Yarden and his student Maicol Mancini discovered what happens to cancer cells when they are exposed to the receptor-blocking antibody.
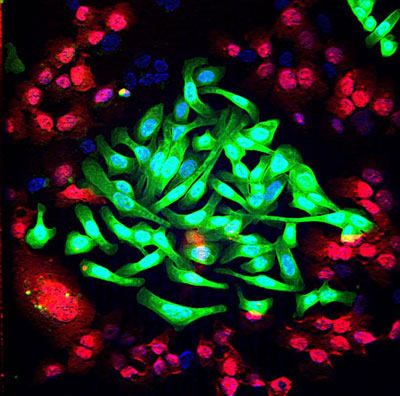
Researchers found that sibling growth receptors appeared on the cell membrane
“The blocked receptor has ‘siblings’ – other receptors that can step up to do the job,” says Yarden. Indeed, the team found that when the main receptor (EGFR) continued to be blocked, one of the cell’s communication networks was rerouted, causing the siblings to appear on the cell membrane instead of the original receptor. The finely-tuned antibody did not block these, and thus the cancer cells were once again “in business.” The researchers uncovered the chain of protein communication in the new network that ultimately leads to appearance of the sibling growth receptors. This new network may overcompensate for the lack of the original receptor, making it even worse than the original. In addition, the team found that the rewired network sometimes included the participation of another molecule, known as receptor tyrosine kinase MET, which specifically binds to one of the siblings. This signalling molecule is often found in metastatic cancers.
Once the researchers discovered how the blockade was breached, they set out to erect a better line of defense. Yarden and his team created new monoclonal antibodies that could target the two main growth receptor siblings, named HER2 and HER3. The idea was to give all three antibodies together – the two new ones and the original anti-EGFR antibody – to pre-empt resistance to the treatment. Indeed, in isolated cancer cells, applying the triple treatment prevented them from completing the rewiring necessary for continuing to receive growth signals.
Using the three-pronged approach, tumour growth was almost completely arrested in mouse models
Next the team tried the three-pronged approach on mouse models of lung cancer that had the secondary, resistance mutation. In these mice, the tumour growth was almost completely arrested. More importantly, further research showed that this treatment reined in the growth of the tumour while leaving healthy cells alone.
Although much more research is required before the triple-treatment approach makes it to the clinic, Yarden is hopeful that it will change not only the treatment protocol for lung cancer, but our understanding of the mechanisms of drug resistance. “Treatment by blocking a single target can cause a feedback loop that ultimately leads to a resurgence of the cancer,” he says. “If we can predict how the cancer cell will react when we block the growth signals it needs to continue proliferating, we can take preemptive steps to prevent this from happening.”
The research appears in the journal Science Signaling.
Related topics
Oncology
Related organisations
Cancer Research, Weizmann Institute of Science