Protein therapy could be used to improve heart function after cardiac arrest
Posted: 2 January 2020 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have shown that a protein therapy has been successful in pre-clinical models at improving the quality of scar tissue after heart attacks, leading to better overall heart function.
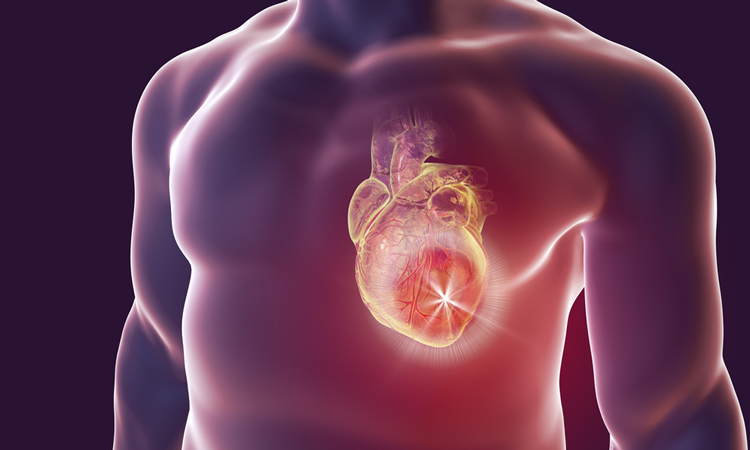
A new study has demonstrated that a protein therapy can improve the outcome for patients following a heart attack.
The research was conducted at the Westmead Institute for Medical Research (WIMR) and the University of Sydney, both Australia.
The team revealed that recombinant human platelet-derived growth factor-AB (rhPDGF-AB) was successful at improving the quality of scar tissue in a large animal model, leading to the formation of new blood vessels in the heart and reduced rates of arrhythmia.
Although the researchers say that the protein therapy treatment did not affect overall scar size, rhPDGF-AB led to increased scar collagen fibre alignment and strength, resulting in improved heart function after the heart attack.
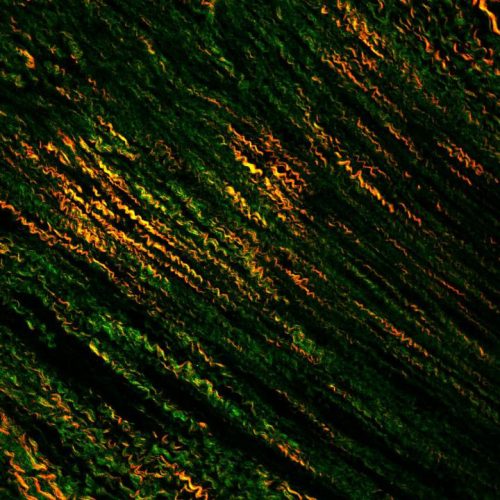
2-photon microscopy image showing “straightening of heart attack scars” (credit: Robert D Hume).
Corresponding author and leader of the research team, Associate Professor James Chong, said: “This is an entirely new approach with no current treatments able to change scar in this way. By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”
Treatments available at present aim to restore blood and the oxygen supply to the heart as quickly as possible to reduce scarring. While this improves clinical outcomes, up to a quarter of patients experiencing their first heart attack will develop heart failure within one year.
“Some further animal studies are required to clarify safety and dosing. Then we can start looking towards clinical trials in humans very soon. rhPDGF-AB is clearly a promising therapeutic option and could potentially be used alongside existing treatments to improve heart attack patient outcomes and survival rates,” concluded Chong.
The findings were published in Science Translational Medicine.
Related topics
Protein, Research & Development, Targets
Related conditions
Heart attack
Related organisations
Sydney University, Westmead Institute for Medical Research (WIMR)
Related people
James Chong