IL-1β produced by pancreatic cancer cells suppresses immune attack on tumours
Posted: 10 January 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Researchers have discovered that pancreatic cancer cells secrete IL-1β to suppress the immune system and suggest antibody treatments as a therapy for pancreatic ductal adenocarcinoma.
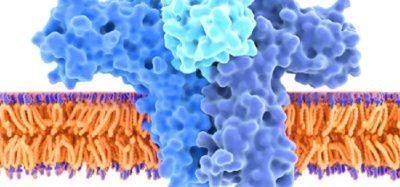
A study has revealed that pancreatic cancer cells produce and release interleukin-1β (IL-1β), an immune signalling protein that stops immune response and promotes the growth of pancreatic ductal adenocarcinoma (PDA).
The research was led by New York University (NYU) Grossman School of Medicine, US.
Researchers found that blocking the action of IL-1β using anti-IL-1β antibodies caused a 32 percent decrease in PDA tumour growth. They then experimented further, combining anti-IL-1β antibodies with an approved antibody therapy that inhibits the PD-1 checkpoint protein.
The PD-1 checkpoint typically protects host tissue from autoimmune strikes but is also frequently hijacked by cancer to stop cancer-killing CD8 T-cell attacks. Checkpoint inhibitors counter this effect, promoting CD8 T-cell infiltration into tumours.
So far, checkpoint inhibitors, although effective in many cancers, have been unsuccessful against PDA with response rates as low as three percent in some trials. This is supposedly because of poor CD8 T-cell infiltration and immune suppression. By combining anti-IL-1β antibodies and anti-PD-1 antibody treatment, the current study doubled the infiltration of T cells into tumours and increased the anti-tumour activity of PD-1 blockade by 40 percent.
“By engineering mice with versions of PDA that lack the IL-1β gene, we found for the first time that pancreatic cancer cells produce IL-1β and that it is essential for the continued growth of PDA tumours,” says Dr Dafna Bar-Sagi, study senior author, Vice Dean for Science and Chief Science Officer for NYU Langone Health. “Blocking IL-1β with an antibody treatment may represent another way to make pancreatic tumours vulnerable to the immune system, with the potential to significantly increase the effectiveness of checkpoint inhibitors if combined.”
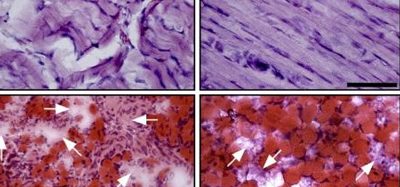
The research team also found that higher IL-1β production caused nearby pancreatic stellate cells to increase production of structural proteins such as collagen. The overgrowth of fibrous tissue, which commonly occurs near pancreatic tumours, is called desmoplasia and has been linked to treatment resistance.
Active stellate cells also triggered production of signalling proteins that attract macrophages into tumours, where they then convert them to M2 macrophages which suppress immune reactions. Experiments confirmed that higher IL-1β and M2 macrophage levels, in combination with desmoplasia, reduced the ability of CD8 T cells to infiltrate tumours.
“This work provides strong evidence that blocking the action of IL-1β enables T cells to better penetrate tumours and kill cancer cells, mechanisms with potential to overcome the limitation of currently available immunotherapies in the treatment of pancreatic cancer,” concluded Shipra Das, first author and a member of Bar-Sagi’s lab at the time of the study.
Study published in Cancer Research.
Related topics
Antibodies, Disease Research, Drug Discovery, Drug Targets, Oncology
Related conditions
Pancreatic cancer, pancreatic ductal adenocarcinoma (PDA)
Related organisations
New York University (NYU) Grossman School of Medicine
Related people
Dr Dafna Bar-Sagi, Shipra Das