New class of CAR T cells combat previously “untargetable” cancer drivers
Posted: 4 November 2021 | Anna Begley (Drug Target Review) | No comments yet
The peptide-centric chimeric antigen receptors killed neuroblastoma cells in mice and could potentially expand the pool of immunotherapeutic targets.
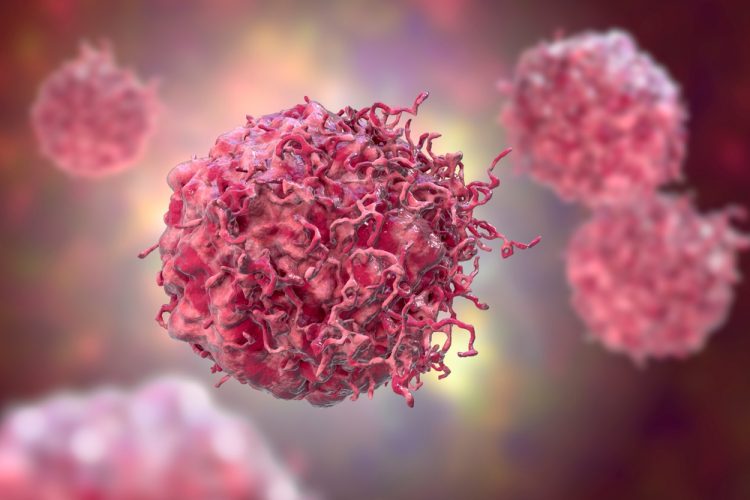
In a breakthrough for the treatment of aggressive solid cancers, researchers at Children’s Hospital of Philadelphia (CHOP), US, have developed a novel cancer therapy involving chimeric antigen receptors (CARs) that targets proteins inside cancer cells that are essential for tumour growth and survival but have previously been difficult to target. The discovery could open the door to treating a broader array of cancers with immunotherapy as well as applying each therapy across a greater proportion of the population.
NEWS: Targeting channel in cell lysosome could selectively kill cancer cells – READ HERE
Neuroblastoma is an explosively aggressive paediatric cancer that is driven by modifications of gene expression that promote uncontrolled tumour growth. Historically, neuroblastoma has been treated with chemotherapy, surgery, and radiation therapy, however patients often relapse with forms of the disease that are chemotherapy resistant. Additionally, the low mutational burden of the cancer combined with its low major histocompatibility complex (MHC) expression, have made it difficult to target with immunotherapies.
The researchers hypothesised that some of the peptides presented on the surface of neuroblastoma tumour cells come from proteins that are essential for tumour growth and survival and could be targeted with synthetic CARs. These peptide-centric CARs (PC-CARs) would allow for direct targeting and killing of tumour cells.
In the study, detailed in Nature, the team stripped MHC molecules off neuroblastoma cells and determined which peptides were present and used a large genomic dataset to determine which peptides were unique to neuroblastoma and not expressed by normal tissues. They subsequently prioritised peptides that were derived from genes essential to the tumour and had characteristics required to engage the immune system. To identify any potential antigens that might have cross reactivity with normal tissue, they filtered the remaining tumour peptides against a database of MHC peptides on normal tissues, removing any peptide with a parent gene represented in normal tissue.
Using this multi-omics approach, the researchers pinpointed an unmutated neuroblastoma peptide that is derived from PHOX2B, a neuroblastoma dependency gene and transcriptional regulator. The researchers developed a PC-CAR targeting this peptide and showed that these PC-CARs recognised the tumour-specific peptide on different HLA types, suggesting that the treatment could be applied to patients of diverse genetic lineages.
The team then tested the PC-CARs in mice and found that the treatment led to complete and targeted elimination of neuroblastoma tumours. “We are excited about this work because it allows us to now go after essential cancer drivers that have been considered ‘undruggable’ in the past. We think that PC-CARS have the potential to vastly expand the pool of immunotherapies and significantly widen the population of eligible patients,” concluded senior author John Maris.
Related topics
Drug Development, Drug Targets, Genetic Analysis, Genomics, Immuno-oncology, In Vivo, Oncology, Target Molecule, Targets, Therapeutics
Related conditions
Neuroblastoma
Related organisations
Children's Hospital of Philadelphia (CHOP)
Related people
John Maris