UCI study points to new treatments to limit effects of Alzheimer’s
Posted: 1 March 2016 | Victoria White | No comments yet
Using pexidartinib to flush away the inflammatory cells produced in reaction to beta-amyloid plaques, scientists restored memory function in test mice…
Using a drug compound created to treat cancer, neurobiologists have disarmed the brain’s response to the distinctive beta-amyloid plaques that are the hallmark of Alzheimer’s disease.
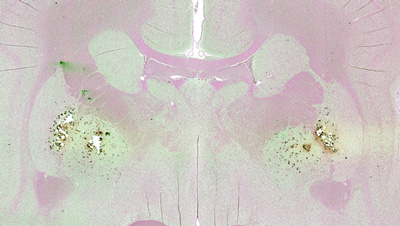
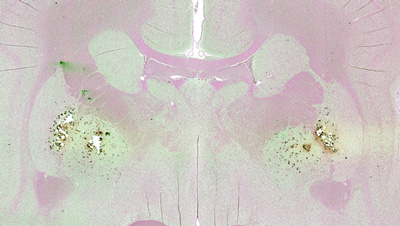
Kim Green and colleagues from University of California, Irvine‘s Institute for Memory Impairments and Neurological Disorders found that flushing away the abundant inflammatory cells produced in reaction to beta-amyloid plaques restored memory function in test mice. Their study showed that these microglia contribute to the neuronal and memory deficits seen in this neurodegenerative disease.
“Our findings demonstrate the critical role that inflammation plays in Alzheimer’s-related memory and cognitive losses,” said Green, an assistant professor of neurobiology & behaviour. “While we were successful in removing the elevated microglia resulting from beta-amyloid, further research is required to better understand the link among beta-amyloid, inflammation and neurodegeneration in Alzheimer’s.”
The neurobiologists treated Alzheimer’s disease model mice with a small-molecule inhibitor compound called pexidartinib, or PLX3397, which is currently being used in several Phase 2 oncology studies and a Phase 3 clinical trial to treat a benign neoplasm of the joints.
Pexidartinib blocks signalling of microglial surface receptors
The inhibitor works by selectively blocking signalling of microglial surface receptors, known as colony-stimulating factor 1 receptors, which are necessary for microglial survival and proliferation in response to various stimuli, including beta-amyloid. This led to a dramatic reduction of these inflammatory cells, allowing for analysis of their role in Alzheimer’s. The researchers noted a lack of neuron death and improved memory and cognition in the pexidartinib-treated mice, along with renewed growth of dendritic spines that enable brain neurons to communicate.
Green said that although the compound swept away microglia, the beta-amyloid remained, raising new questions about the part these plaques play in Alzheimer’s neurodegenerative process.
In healthy tissue, microglia act as the first and main form of immune defense in the central nervous system. But in a disease state, such as Alzheimer’s, microglia appear to turn against the healthy tissue they were originally assigned to protect, causing inflammation in the brain. The beta-amyloid plaques in brain areas related to Alzheimer’s disease are rich with these rogue microglia, Green added.
“Our work is telling us that these cells may contribute to the disease process, and targeting them with such specific drugs is a promising new approach,” he said.
Related conditions
Alzheimer’s disease
Related organisations
UC Irvine



