Advancing personalised medicine with a cholangiocarcinoma model
Posted: 23 January 2024 | Drug Target Review | No comments yet
A patient-specific organ-on-a-chip model of cholangiocarcinoma, with its tumour microenvironment, helps to predict therapy response.
For the first time, a patient-specific organ-on-a-chip model of a biliary tract cancer called cholangiocarcinoma, complete with its tumour microenvironment, has been made by Dr Ana Lleo De Nalda from the Humanitas University, Dr Marco Rasponi from Politecnio di Milano and Dr Guido Torzilli’s group from the IRCCS Istituto Clinico Humanitas.
Dr Lleo and Dr Rasponi explained: “The ultimate goal of the device is to accelerate research on cholangiocarcinoma by providing a new laboratory model that better mimics what we observe in patients. At the same time, it will help advancing precision medicine, since it could be potentially used as a personalised drug-testing platform, helping predict patients’ response to therapies.”
Cholangiocarcinoma
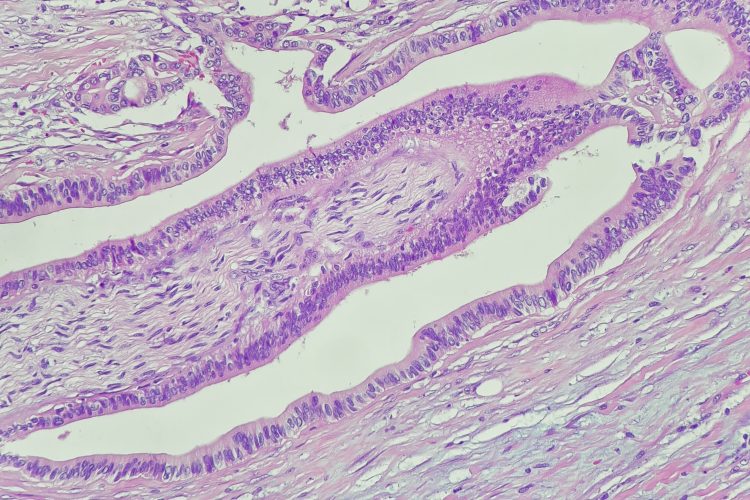
Cholangiocarcinoma is a rare cancer of the liver, deriving from a malignant transformation of cholangiocytes, the cells lining the biliary tract.
Patients show limited symptoms so the disease is frequently diagnosed at an advanced stage. Treatments are often ineffective because, at the time of diagnosis, only 10 to 30 percent of patients are eligible to undergo surgical removal of the tumour.
Dr Lleo stated: “Precisely because of the reduced therapeutic options and high mortality of cholangiocarcinoma, we need new in vitro models that can recapitulate the characteristics of the disease and in particular the interaction between tumour cells and cells of the immune system, which play a key role in its progression and response to drugs.”
Personalised medicine
The microfluidic chip is only a few centimetres in size. “Inside the device, in the micrometre channels realised using advanced photolithographic techniques, we seeded cancer cells sampled from patients affected by cholangiocarcinoma. The cells successfully reproduced the tumour architecture in vitro,” detailed Dr Rasponi.
The researchers, to add complexity to the model and improve its reliability, seeded fibroblasts, T lymphocytes and endothelial cells into it. Then, they conducted a series of experiments to demonstrate that the device shows what is observed in individual patients, in terms of T-cell activation that correlates with tumour infiltration, and in terms of therapeutic response to different drugs, based on the characteristics of cancer recurrence.
“The next steps will be to further optimise and improve the device, both as a research model and as a personalised drug-testing platform: we want to add cells of innate immune system, such as macrophages, which play an important role in tumour progression, and introduce micro-pumps that can mimic blood flow and vascularisation,” concluded Dr Lleo and Dr Rasponi.
“We also need to test it on larger groups of patients, to confirm its ability to recapitulate the phenomena we observe in the clinical setting.”
This study was published in the Journal of Hepatology Reports.
Related topics
Cancer research, Organ-on-a-Chip, Personalised Medicine
Related conditions
Cancer Research, Cholangiocarcinoma.
Related organisations
Humanitas University, IRCCS Istituto Clinico Humanitas, Politecnio di Milano