How PD-1 promotes Merkel cell carcinoma progression
Posted: 23 January 2024 | Drug Target Review | No comments yet
Inhibiting mTOR signalling and neutralising mtROS suppressed MCC-PD-1-mediated tumour proliferation in mice.
Researchers from the Brigham and Women’s Hospital have identified a novel mechanism through which programmed cell death 1 (PD-1) promotes Merkel cell carcinoma (MCC) progression. Their findings could optimise immune checkpoint therapy regimens and improve MCC patient outcomes.
PD-1is a key target for immune checkpoint inhibitor therapies that block its signalling and boost T-cell activity. PD-1 inhibitors have been approved for treating various types of cancer. However, PD-1 functions can vary between different cell and cancer types, either promoting or suppressing disease progression.
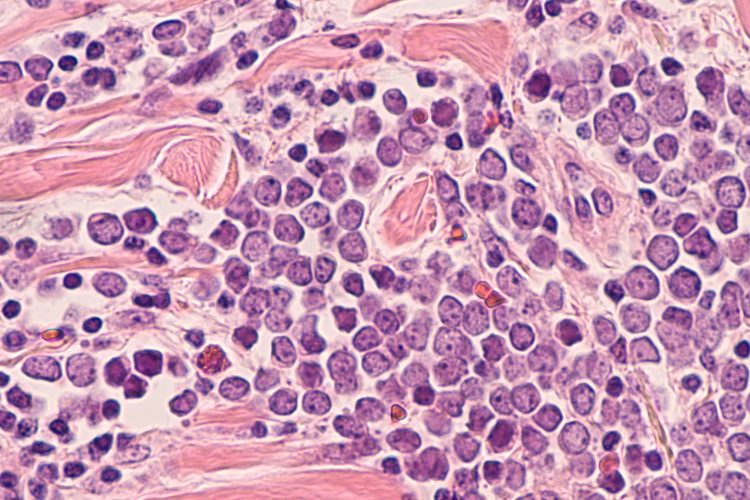
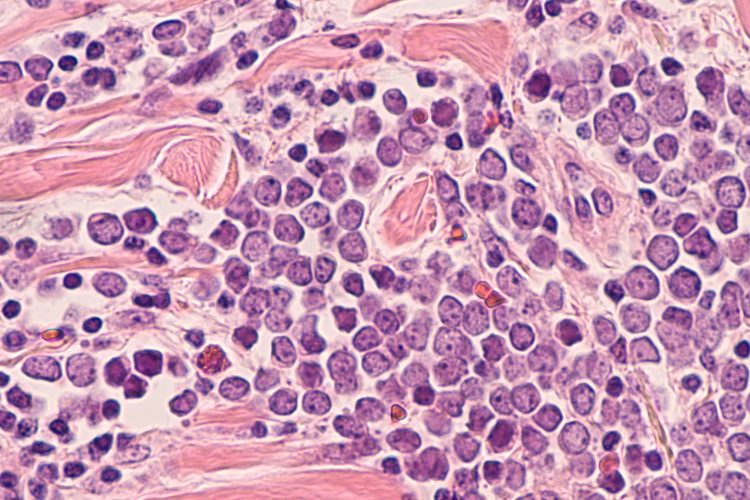
MCC, a rare and aggressive form of skin cancer, responds well to immune checkpoint inhibitor therapy, but it was previously unknown if MCC cells express PD-1 themselves and how exactly cancer cell-intrinsic PD-1 contributes to tumour growth.
The researchers, through a series of experiments, demonstrated PD-1 expression on MCC cells in preclinical models and patient tumour samples. They discovered that MCC-PD-1 receptor binding to its ligands accelerated tumour growth by activating the mammalian target of rapamycin (mTOR) pathway and generating mitochondrial reactive oxygen species (mtROS) to promote MCC growth.
Then, the team demonstrated that inhibiting mTOR signalling and neutralising mtROS suppressed MCC-PD-1-mediated tumour proliferation in mice. These findings could aid the development of new treatments to stop MCC progression, even in patients lacking T-cell immunity.
Corresponding author Dr Tobias Schatton, from the Department of Dermatology, detailed: “For the first time, our work identifies PD-1 as an MCC-intrinsic receptor that promotes tumour growth via downstream mTOR signalling and mitochondrial reactive oxygen species production…Targeting this tumour-intrinsic PD-1 signalling network could help optimise immune checkpoint therapy regimens and improve MCC patient outcomes.”
This was published in Science Advances.
Related topics
Cancer research, T cells
Related conditions
Cancer Research, Merkel cell carcinoma
Related organisations
Brigham and Women's Hospital
Related people
Dr Tobias Schatton (Brigham and Women’s Hospital)