CAR-NK cells: promising for cancer therapy
Posted: 17 November 2023 | Aleta Pupovac (Carthetics), Dr Huimin Cao (Cartherics), Professor Alan Trounson (Cartherics) | No comments yet
The suitability of NK cells for cancer therapy has been challenged by some investor and business interests because of limited efficacy data, is this a valid belief at the present stage of development of the immune therapy field?
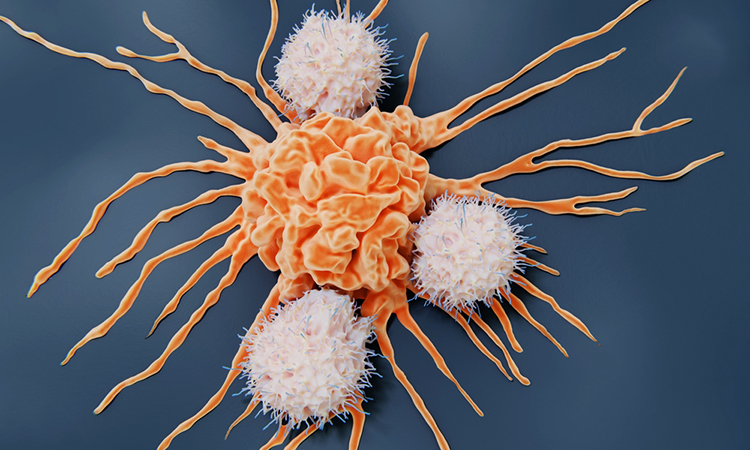
NK cells are among the front line of protection from infected and abnormal cells as part of the ‘innate immune response’. They recognise ‘cell stress molecules’ on the surface of infected, old, injured and cancerous cells without the need for complex pre-stimulation signals of the adaptive immune system (eg, T cells). They do not induce ‘graft versus host’ disease when transplanted for allogeneic therapy and there appears little sign of immune rejection.
NK cells can be readily extracted from umbilical cord blood or peripheral blood of adult donors. They may also be derived from induced pluripotent stem cells (iPSCs) made from blood leukocytes or cells of adult tissues. iPSCs are pluripotent, immortal, and may be directed into any cell of the body. NK cells can be manufactured in great abundance from iPSCs in three broad stages: (i) patterning of iPSC into CD34+ cells in 3D bioreactors; (ii) differentiation into NK cells; (iii) numerical expansion and functional maturation under a milieu of growth factors and cytokines. iPSCs may also be gene edited to insert chimeric antigen receptors (CARs) and other enhancers of function and block genes that are part of the inhibition of immune function (frequently used by solid tumours to block killing function of immune cells).
These cells can be clonally derived after gene editing, making them ideal for selecting the desired gene edits and ensuring there are no off-target effects or mutations. The relative ease and lower cost of manufacture (potentially a few thousand dollars) compared to autologous T cell therapies (hundreds of thousands of dollars), coupled with their functional attributes and safety profile, make NK cells an attractive therapeutic option for cancer patients, but surprisingly this is not universally recognised.
Peripheral blood NK cells have been used in allogeneic cancer therapies and shown to be safe. Up until 2023 around 600 NK cell clinical trials have been reported and some 200 are clinically active and still recruiting patients. We have analysed 74 studies where clinical data are available from publications, conference reports and company news releases. Summarising the information:
- 36/74 (48 percent) were for advanced solid tumours and the remainder were for haemopoietic (blood) malignancies. The vast majority (65/74; 88%) of those trials involved NK cells without CARs; while only 12 percent were CAR-NK studies. Only three of the CAR-NK studies were for the treatment of solid tumours.
- The non-CAR-NK studies showed very good safety data when compared to neurological and cytokine storm responses reported for CAR-T cell trials. By themselves, the NK cells showed limited efficacy, but anti-tumour efficacy was observed with co-treatment regimens (eg, monoclonal antibodies, haematopoietic stem cell transplants, whole body irradiation) and multiple dosing (tolerated well by patients).
- CAR-NK cell trials only commenced in 2017 and most are still recruiting patients. The limited data available show excellent on-target cancer killing efficiencies without compromise of the safety profile seen in non-CAR-NK cell clinical trials reported to date.
Four CAR-NK studies, where efficacy data are available, are described in more detail below:
Study 1: NKG2D-CAR-NK (patient derived or donor NK cells) for metastatic colorectal cancer. Three patients were treated with 2-6 doses of 2×107 to 2×109 cells. All three patients had a significant decrease of tumour load in ascites fluid and these tumour cells became undetectable by the end of treatment. The study sponsor and clinical site is the Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China (NCT03415100).
Study 2: NKX101 NKG2D-CAR-NK (allogeneic donor CAR-NK cells) for acute myeloid leukaemia (AML). Twenty-four patients were treated with 2-3 doses of 1X108 to 1.5X109 cells. Of reports available, 4/18 patients had complete recovery. Of those who had Flu/Ara-C pre-conditioning, 3/6 had complete recovery. The study is sponsored by Nkarta Inc. and clinical sites are located across the United States, including Colorado, Florida, Georgia, Illinois, Ohio, Tennessee and Texas (NCT04623944).
Study 3: FT596 CD19-CAR-iNK (iPSC derived CAR-iNK cells) for B cell lymphoma. Single dose of 3X107 to 9X108 cells. 98 patients enrolled, of which data were reported for 26. 18/26 achieved a response. At the highest dose, 9/12 patients had a complete response. The study is sponsored by Fate Therapeutics and clinical sites are located across the United States, including Illinois, Minnesota, Missouri, New York, Tennessee, Texas and Washington (NCT04245722).
Study 4: CD19-CAR-NK cells (cord blood derived CAR NK cells) for CD19+ Non-Hodgkin’s lymphoma. 44 patients enrolled, of which data has been reported for 11. They were treated with a single dose of 1X105 to 1X107/kg. After a median follow-up of 13.8 months, 8 (73 percent) had a response (rapid within 30 days). CAR-NK cells expanded and persisted for at least 12 months. The study sponsor and clinical site is the University of Texas MD Anderson Cancer Center, Houston, Texas, United States (NCT03056339).
Given that the available evidence for CAR-NK studies show both safety and reasonable efficacy at reducing targeted cancers, it is not valid to conclude that NK cells are not an effective therapy for cancer. Indeed, the likely progress from these very encouraging studies of a new cohort of new clinical trials, are likely to provide a major shift towards innovative CAR-NK therapies.
About the authors


Publications Officer, Cartherics
Aleta is a cell biologist and immunologist who is passionate about translational science. She obtained her PhD from the University of Wollongong in 2015 and gained extensive research experience as a postdoctoral fellow at Swinburne University of Technology, CSIRO, and Monash University, in the fields of immunology and tissue engineering. As an early career scientist, Aleta has contributed to the scientific community with the publication of 15 papers. Currently, she is the Publications Officer at Cartherics, a biotech company specialising in the creation of Chimeric Antigen Receptor (CAR)-T and CAR-NK cell therapies, which are transforming the landscape of cancer treatment.


CEO, Executive Director, Cartherics
Alan is the past President of the Californian Institute for Regenerative Medicine (2007-2014), the Californian state’s $3 billion stem cell agency driving research in stem cell biology and facilitating the translation of stem cell discoveries into clinical therapies. He was a pioneer of human in vitro fertilisation (IVF) (1977-1996) and led the Australian team for the discovery of human embryonic stem cells in the late 1990’s and was awarded the first Australian Biotechnology of Excellence in 2003. He was the founding CEO of the Australian Stem Cell Centre.
Alan founded the Monash Immunology and Stem Cell Laboratories at Monash University (2004-7). He is presently the founding CEO/President of the start-up company Cartherics Pty Ltd., developing immune stem cell therapies for treating ovarian and gastric cancer. Alan is Emeritus Professor Monash University and Distinguished Scientist, Hudson Institute for Medical Research, Clayton, Victoria, Australia.


Senior Research Fellow, Cartherics
Dr Madeline Cao received her MD in 2010 and practiced at Institute of Hematology & Blood Diseases Hospital in Tianjin, China. Then she moved to Australia to expand her research interests on hematopoiesis, including a PhD and subsequent postdoctoral research in hematopoietic stem cells and their residential niche. In 2019, she joined Cartherics focusing on the science underpinning induced pluripotential stem cell differentiation to natural killer cells, and how to manufacture them. In conjunction of clinical practise and research experience, Dr Cao has developed a strong expertise in stem cell biology and a huge passion in utilizing stem cells to develop innovative therapeutic strategies to help patients fight cancer.
Related topics
Disease Research, Immuno-oncology, Immunology, Immunotherapy
Related organisations
Cartherics