Cell transplant that responds to designer drugs treats Parkinson’s disease
Posted: 28 April 2016 | Victoria White, Digital Content Producer | No comments yet
Su-Chun Zhang created two related cell types. When the cells detect the designer drug, one type ramps up production of dopamine; the other chokes it off…
A University of Wisconsin-Madison neuroscientist has inserted a genetic switch into nerve cells so a patient can alter their activity by taking designer drugs that would not affect any other cell.
The cells in question are neurons and make the neurotransmitter dopamine, whose deficiency is the culprit in Parkinson’s disease.
Dopamine replacement, a standard therapy for Parkinson’s disease, usually loses its effect with time and, with the advent of stem cell technology, biomedical researchers have explored the notion of making dopamine-producing cells in the lab for transplant. While doctors have tested dopamine cell transplants, the therapy often fails when the transplanted cells make either too much or too little of the essential neurotransmitter.
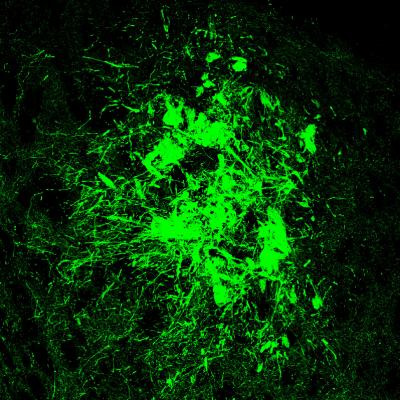
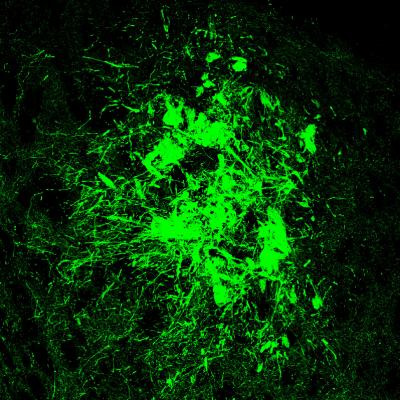
In a new study, Su-Chun Zhang, a professor of neuroscience at the UW-Madison Waisman Center, created two related cell types. When they detect the designer drug, one type ramps up production of dopamine; the other chokes it off.
Zhang and colleagues grew the specialised nerve cells from human embryonic stem cells. Their behavioural tests, designed to show when the Parkinson’s symptoms abated in the mice, confirmed that both the “up” and “down” switches performed as anticipated. The results suggest that it may one day be possible to resume dopamine neuron transplants to assist Parkinson’s disease patients.
Wider applications
But the ability to transplant cells that respond to regulatory drugs could have much wider applications, says Zhang: “This is the first proof of principle, using Parkinson’s disease as the model, but it may apply to many other diseases, and not just neurological diseases.”
Cells tend to have quite specific actions, and the ability to control them with benign drugs could find other uses, he says. In diabetes, for example, “perhaps the beta cells that secrete insulin could be transplanted, and the patients could control insulin secretion with a designer drug”.
Cell therapy was one of the most touted potential benefits of embryonic stem cells and the stem cells that were later derived from adult tissue (both technologies pioneered at UW-Madison), but few applications have reached the clinic as the technology continues to be refined and made safer. Control is part of the problem, Zhang says: “If we are going to use cell therapy, we need to know what the transplanted cell will do. If its activity is not right, we may want to activate it, or we may need to slow or stop it.”
The mouse study showed both abilities, says Zhang, who anticipates that cells will also be engineered to contain switches that work in both directions.
Several major steps will be needed before the first clinical trial can be started. Despite those hurdles, Zhang considers the discovery one the most exciting in his substantial record of scientific firsts. After the engineered cells are transplanted into the mouse brain, he says, “we can turn them on or off, up or down, using a designer drug that can only act on cells that express the designer receptor. The drug does not affect any host cell because they don’t have that specialised receptor. It’s a very clean system.”
Related topics
Stem Cells
Related conditions
Parkinson's disease
Related organisations
University of Wisconsin-Madison