Controlling cholesterol metabolism in pancreatic cancer cells reduces metastasis
Posted: 4 May 2016 | Victoria White, Digital Content Producer | 1 comment
The findings of a new study suggest a class of drugs previously developed to treat atherosclerosis could be repurposed for treatment of pancreatic cancer…
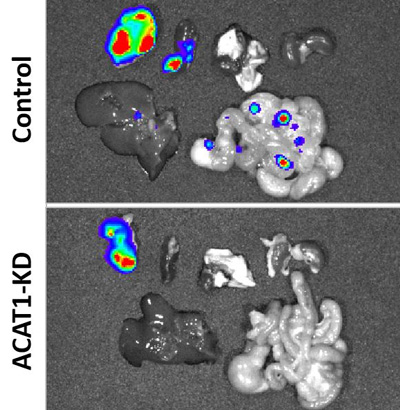
Researchers have shown how controlling cholesterol metabolism in pancreatic cancer cells reduces metastasis to other organs, pointing to a potential new treatment. Findings showed a higher number of metastatic lesions in organs of untreated and treated mice, shown at top and bottom, respectively. CREDIT: Purdue University image/Junjie Li
Researchers have shown how controlling cholesterol metabolism in pancreatic cancer cells reduces metastasis, pointing to a potential new treatment using drugs previously developed for atherosclerosis.
The findings suggest a class of drugs previously developed to treat atherosclerosis could be repurposed for treatment of pancreatic cancer and other forms of cancer. Atherosclerosis is the buildup of fats, cholesterol and other substances in arteries, restricting blood flow.
The researchers found accumulations of the compound cholesteryl ester in human pancreatic cancer specimens and cell lines, demonstrating a link between cholesterol esterification and metastasis. Esterification is a biochemical process that allows cholesterol to be stored in cells. Excess quantities of cholesterol result in cholesteryl ester being stored in lipid droplets within cancer cells.
“The results of this study demonstrate a new strategy for treating metastatic pancreatic cancer by inhibiting cholesterol esterification,” said Jingwu Xie, the Jonathan and Jennifer Simmons Professor at the Indiana University School of Medicine and a researcher at the Indiana University Melvin and Bren Simon Cancer Center. The new study involved researchers at Purdue University and Indiana University.
Avasimibe suppressed tumour size and largely reduced tumour growth rate
Findings show that drugs like avasimibe, previously developed for treatment of atherosclerosis, reduced the accumulation of cholesteryl ester. The disease usually kills within a few months of diagnosis. It is hoped the potential new treatment might extend life of pancreatic cancer patients for a year, said Ji-Xin Cheng, a professor in Purdue University’s Weldon School of Biomedical Engineering and Department of Chemistry.
The accumulation of cholesteryl ester is controlled by an enzyme called ACAT-1, and findings correlated a higher expression of the enzyme with a poor survival rate for patients. The researchers analysed tissue samples from pancreatic cancer patients and then tested the drug treatment in a type of laboratory mice referred to as an orthotopic mouse model.
Imaging showed a decrease of the number of lipid droplets, and Raman spectral analysis verified a significant reduction of cholesteryl ester in the lipid droplets, suggesting that avasimibe acted by blocking cholesterol esterification. The drug did not induce weight loss, and there was no apparent organ toxicity in the liver, kidney, lung and spleen, Cheng said.
Findings also showed that blocking storage of cholesteryl ester causes cancer cells to die, specifically due to damage to the endoplasmic reticulum, a workhorse of protein and lipid synthesis.
“By using avasimibe, a potent inhibitor of ACAT-1, we found that pancreatic cancer cells were much more sensitive to ACAT-1 inhibition than normal cells,” he said.
Additional research confirmed that the anti-cancer effect of avasimibe is specific to ACAT-1 inhibition. The researchers performed various biochemical assays and “genetic ablation” to confirm the drug’s anti-cancer effect.
“The results showed that avasimibe treatment for four weeks remarkably suppressed tumour size and largely reduced tumour growth rate,” said Timothy Ratliff, the Robert Wallace Miller Director of Purdue’s Centre for Cancer Research. “Metastatic lesions in lymph nodes and distant organs also were assessed at the end of the study. A much higher number of metastatic lesions in lymph nodes were detected in the control group than the avasimibe-treated group.”
Each mouse in the control group showed at least one metastatic lesion in the liver. In contrast, only three mice in the avasimibe treated group showed single lesion in liver.
Related conditions
Atherosclerosis, Pancreatic cancer
Related organisations
Indiana University, Purdue University



My congratulations! Using of known medicines for treatment of other diseases is very attractive. If clinical trial will show similar results, avasimibe may be rapidly adopted to clinical practice.
Kind regards,
Eugeniy Smorodin, PhD.