Reducing drug resistance in acute myeloid leukaemia patients
Posted: 6 February 2024 | Drug Target Review | No comments yet
Researchers conducted a proteogenomic characterisation and found that drug exposure changes drug sensitivity.
Researchers from the Department of Energy’s Pacific Northwest National Laboratory (PNNL) and Oregon Health & Sciences University (OHSU) have made novel findings regarding how drug resistance develops in certain acute myeloid leukaemia (AML) patients. They also elucidate how clinicians could stop or slow this process.
Proteogenomics
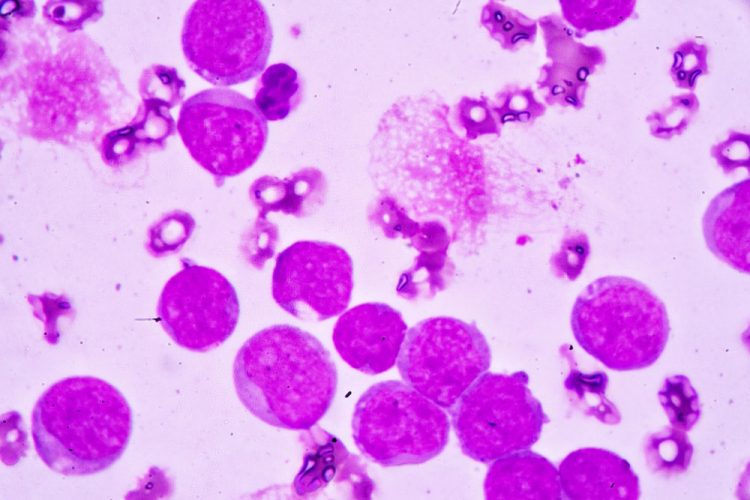
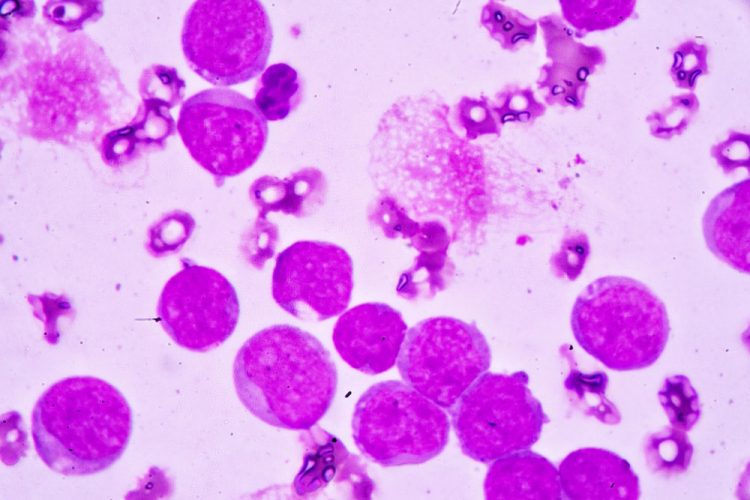
In the new study, a team led by Dr Sara Gosline, a data scientist and computational biologist at PNNL, conducted an extensive study of the protein activity in 210 AML patients. Nearly half a million pieces of proteins from over 9,000 proteins in patients’ blood samples were measured. These findings were then combined with data already known about AML, such as the genes and mutations involved, the molecular messengers that indicate which genes are active, and the effects of 46 drugs on AML patients, as well as information about how the disease progressed in those patients.
Dr Gosline and her colleagues utilised artificial intelligence, employing several machine learning algorithms to make sense of the data. She explained: “We were able to look at patterns of drug responses in hundreds of people by including protein and gene measurements together, and this gave us a level of detail that hasn’t been possible in prior studies…This is a great example where we are able to put our growing knowledge of protein signalling and machine learning models to benefit patients in the future.”
Drug resistance
One finding was notable, suggesting a potential method of delaying drug resistance for some patients. Quizartinib, approved last year to treat AML, was shown to change how cancer cells respond to other drugs often used in combination to treat patients.
Dr Gosline commented: “You hit the tumour with one drug and the tumour changes. This is what happens when patients experience drug resistance and the medicines stop working. Our study helps us understand exactly how this happens and what might be done in response. Which medication is best to turn to?”
Study author Dr Cristina Tognon, associate research professor and scientific director of the Druker Laboratory at OHSU elaborated: “When you treat a tumour with a drug, you are putting pressure on the tumour cells as they try to figure out a way to escape that pressure and survive. It’s a big problem in AML patients. What’s even more difficult is that in AML, there are many mutations at work; the disease doesn’t come in just one flavour.”
The scientists concentrated on 147 proteins and specific molecular locations called phosphosites that have a crucial part in determining which proteins are turned on or off, and identified four proteogenomic subtypes that correspond to AML drug response. Patients whose samples placed them in one of the groups had a better prognosis than the others, surviving over five years. This information would be very useful in the clinic, enabling patients to avoid aggressive therapies that bring severe side effects if they have a good prognosis, yet ensuring patients who have the worst prognosis are treated as aggressively as possible.
OHSU’s Dr Jeff Tyner, professor of medicine at the OHSU School of Medicine and Knight Cancer Institute explained this study’s implications for the future: “There is potential for clinical applications to be derived from this work, for example, diagnostics, such as protein biomarkers to predict responses to therapies, and the design of new drug combinations that might outperform current ones.”
This study was published in Cell Reports Medicine.
Related topics
Cancer research, Machine learning, Proteogenomics
Related conditions
acute myeloid leukaemia (AML), Cancer Research
Related organisations
Department of Energy’s Pacific Northwest National Laboratory (PNNL), Oregon Health & Sciences University (OHSU)
Related people
Dr Cristina Tognon (OHSU), Dr Jeff Tyner (OHSU), Dr Sara Gosline (PNNL)