New research shows way to bypass immunotherapy resistance
Posted: 3 January 2025 | Drug Target Review | No comments yet
A study from the University of Alabama at Birmingham reveals that HIF1α plays a crucial role in enabling T cells to kill tumour cells under low-oxygen conditions, providing a potential solution to resistance in immune checkpoint blockade (ICB) therapies.
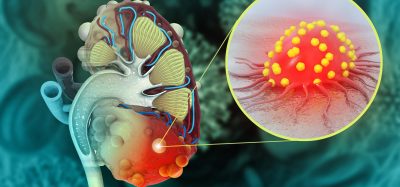
A new study from the University of Alabama at Birmingham (UAB) has revealed a key regulator, HIF1α, that may offer a breakthrough in cancer immunotherapy. Researchers have demonstrated that HIF1α plays a vital role in enabling T cells to kill tumour cells under low-oxygen conditions, known as hypoxia, which is commonly found within tumour microenvironments. The findings could help overcome the resistance that currently reduces the effectiveness of immune checkpoint blockade (ICB) therapies, a treatment used for many advanced cancers.
HIF1α: A key regulator in hypoxic T cells
Immune checkpoint blockades (ICBs) have shown significant promise in treating advanced cancers, but their effectiveness often diminishes due to resistance, particularly when tumour-infiltrating lymphocytes (TILs) are unable to mount an effective attack. These T cells are a crucial part of the immune response, and their ability to kill tumour cells can be hindered by the tumour’s low-oxygen environment. Understanding how to overcome this resistance is essential for improving the clinical outcomes of cancer immunotherapy.
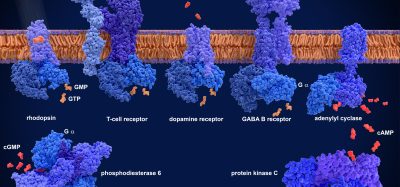
The study, published in Nature Communications, led by Dr Lewis Zhichang Shi and his team, identified HIF1α as a key regulator of interferon gamma (IFN-γ) production in T cells under hypoxic conditions. IFN-γ is a key cytokine that enables T cells to effectively kill tumour cells. Additionally, the research found that HIF1α regulates glycolysis, a metabolic process that allows cells to generate energy in the absence of oxygen – an essential process for IFN-γ induction in hypoxic T cells.
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
New insights into cancer immunotherapy resistance
Under normal oxygen levels (normoxia), IFN-γ induction in T cells is regulated by the enzyme LDHa, a known downstream target of HIF1α. However, the researchers discovered that in hypoxic conditions, HIF1α itself becomes a crucial mediator for both glycolysis and IFN-γ production in T cells.
“Intriguingly, under normal oxygen levels in the body, called normoxia, IFN-g induction and glycolysis in T cells are not mediated by HIF1α, a primary regulator of glycolysis, but by its widely regarded downstream target LDHa, as reported in an early study by another group,” said Shi. “However, it has been unknown, under hypoxia, whether and how HIF1α regulates IFN-γ induction and glycolysis in T cells.”
Using a combination of genetic mouse models, metabolic flux analysis, and pharmacological approaches, the team demonstrated that the deletion of HIF1α in T cells under hypoxic conditions prevented the shift to anaerobic glycolysis and suppressed IFN-γ production. This metabolic shift is crucial for the T cells’ tumour-killing function. Moreover, pharmacological inhibition of glycolysis also hindered IFN-γ production in hypoxic T cells.
Overcoming resistance to immune checkpoint blockade therapy
In an important finding, the researchers showed that stabilising HIF1α in T cells could restore IFN-γ production under hypoxic conditions, overcoming the resistance typically seen in ICB therapies. By supplementing acetate, a metabolite crucial for glycolysis, the researchers were able to bypass the effects of HIF1α deletion, enhancing T cell function in tumour-bearing mice. This strategy, when combined with ICB therapy, resulted in significant suppression of tumour growth.
A new approach to immunotherapy
The study offers hope for enhancing the effectiveness of immunotherapy treatments by addressing the metabolic challenges that impair TIL function in hypoxic tumour environments. By targeting the HIF1α-glycolysis pathway, it may be possible to rejuvenate TILs, allowing them to overcome resistance and effectively combat cancer.
This breakthrough could lead to new therapies that enhance the potency of immune checkpoint blockade treatments, improving outcomes for cancer patients who have previously shown resistance to these therapies.
This study was published in Nature Communications.
Related topics
Biomarkers, Cancer research, Cell Therapy, Cytokines, Drug Discovery, Drug Discovery Processes, Immuno-oncology, Immuno-oncology therapeutics, T cells
Related conditions
hypoxia, Tumour-infiltrating lymphocytes (TILs)
Related organisations
National Institutes of Health (NIH), O’Neal Comprehensive Cancer Center at UAB, University of Alabama at Birmingham (UAB), University of Alaska Fairbanks
Related people
Dr Lewis Zhichang Shi