Nonresponsive NK cells directly impact malaria severity
Posted: 5 October 2018 | Drug Target Review | No comments yet
The failure of natural killer cells (NK cells) to respond to infection explains why malaria causes a worse reaction in some patients than others.
Of the 250 million people who contract malaria every year, in approximately half a million of those it proves fatal. A new study from Massachusetts Institute of Technology (MIT) offers a possible explanation for this different experience. The researchers found that, in some patients, immune cells called NK cells fail to activate the genes necessary to effectively destroy malaria-infected red blood cells.
However, they also showed that they could stimulate NK cells to do a better job of killing infected red blood cells, when grown in a lab dish. This suggests a possible approach for developing treatments that could help reduce the severity of malaria infections in some people – especially children, says Jianzhu Chen, one of the study’s senior authors.
Commenting on the section of the population most vulnerable to the disease, Chen, an MIT professor of biology and member of MIT’s Koch Institute for Integrative Cancer Research, said: “This is one approach to that problem.
“Most of the malaria patients who die are children under the age of five, and their immune system has not completely formed yet.”
Peter Preiser, a professor at Nanyang Technical University (NTU) in Singapore, is also a senior author of the study and the paper’s lead authors are NTU and Singapore-MIT Alliance for Research and Technology (SMART) graduate students Weijian Ye and Marvin Chew.
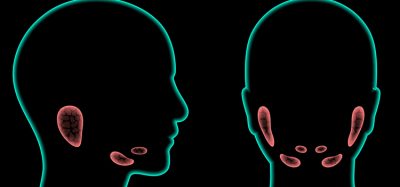
In 2010, Chen and his colleagues engineered strains of mice that produce several types of human immune cells and red blood cells. These “humanised” mice can be used to study the human immune response to pathogens that don’t normally infect mice, such Plasmodium falciparum, the parasite that causes malaria.
A few years later, the researchers used those mice to investigate the roles of NK cells and macrophages in malaria infection. These two cell types are key players in the innate immune system, a nonspecific response that acts as the first line of defence against many microbes. Chen and his colleagues found that when they removed human NK cells from the mice and infected them with malaria, the quantity of parasites in the blood was much greater than in mice with NK cells. This did not happen when they removed human macrophages, suggesting that NK cells are the most important defenders against malaria.
In that study, the researchers also found that in about 25% of the human blood samples they used, the NK cells did not respond to malaria at all. In the new paper, they set out to discover the reason for this. As such, they sequenced the RNA of NK cells before and after they encountered malaria-infected red blood cells, which allowed them to identify a small number of genes that get turned on in malaria-responsive NK cells but not in nonresponsive cells.
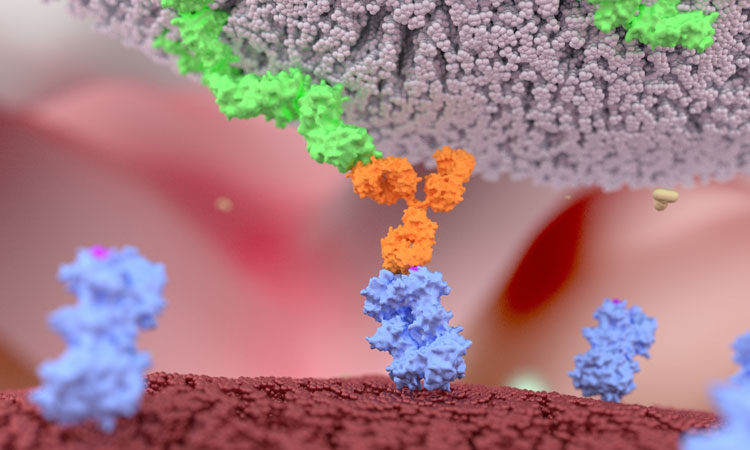
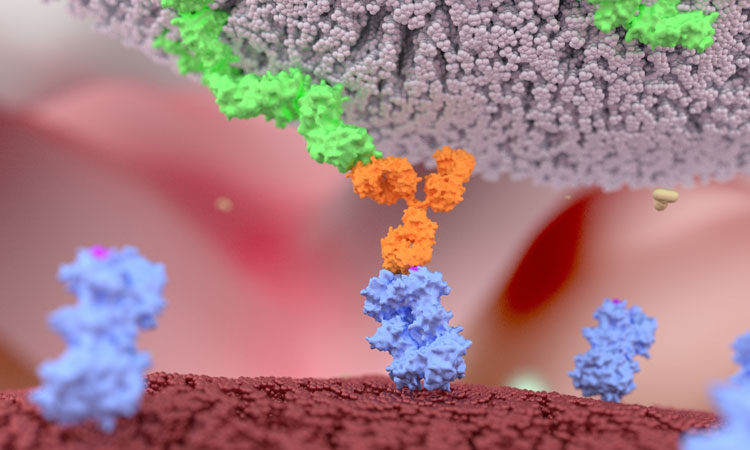
Among these genes was one that codes for a protein called MDA5, which was already known to be involved in helping immune cells such as NK cells and macrophages recognise foreign RNA. Further studies revealed that malaria-infected red blood cells secrete tiny bubbles called microvesicles that carry pieces of RNA from the malaria parasite. The studies also showed that NK cells absorb these microvesicles. If MDA5 is present, the NK cell is activated to kill the infected blood cell.
Nonresponsive NK cells, which have lower levels of MDA5, fail to recognise and kill the infected cells. NK cells are also responsible for secreting cytokines that summon T cells and other immune cells, so their failure to activate also hinders other elements of the immune response.
Chen and his colleagues also showed that they could activate the nonresponsive NK cells by treating them with a synthetic molecule called poly I:C, which is structurally similar to double-stranded RNA. For poly I:C to be effective, the researchers had to package it into tiny spheres called liposomes, which allow it to enter cells in the same manner as RNA-carrying microvesicles.
The researchers also found a correlation between the levels of MDA5 in the NK cells and the disease severity experienced by the patients who donated the blood samples.
Next, they hope to take cells from human patients and use them to further examine this correlation in humanised mice, and also to explore whether treating the mice with poly I:C would have the same beneficial effect they saw in cells grown in a lab dish.
The study appears in the journal PLOS Pathogens.
Related topics
Disease Research, Immunology
Related conditions
Malaria