Scripps scientists make leukaemia cells kill each other
Posted: 20 October 2015 | Victoria White
The surprise finding could lead to a powerful new therapy for leukaemia and possibly other cancers…
Scientists at The Scripps Research Institute (TSRI) have found a way to change leukaemia cells into leukaemia-killing immune cells.
The surprise finding could lead to a powerful new therapy for leukaemia and possibly other cancers.
“It’s a totally new approach to cancer, and we’re working to test it in human patients as soon as possible,” said senior investigator Richard A. Lerner, Institute Professor and the Lita Annenberg Hazen Professor of Immunochemistry at TSRI.
The findings result from the discovery of a rare human antibody.
The Lerner laboratory recently mounted an effort to find therapies for people with certain immune cell or blood factor deficiencies, by looking for antibodies that activate growth-factor receptors on immature bone marrow cells that might induce these bone marrow cells to mature into specific blood cell types. Lerner and his team succeeded in identifying a number of antibodies that activate marrow-cell receptors in this way.
In the process, the scientists noted that some of these receptor-activating antibodies have unexpected effects on marrow cells, causing them to mature into radically different cell types, such as neural cells. The discovery led the team to wonder if they could also use the method to convert cancerous marrow cells (leukaemia cells) into non-cancerous cells.
To find out, the team tested 20 of their recently discovered receptor-activating antibodies against acute myeloid leukaemia cells from human patients. One of these antibodies turned out to have an extraordinary impact on the acute myeloid leukaemia cells.
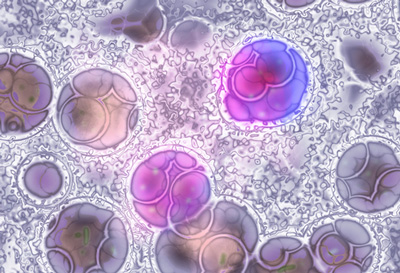
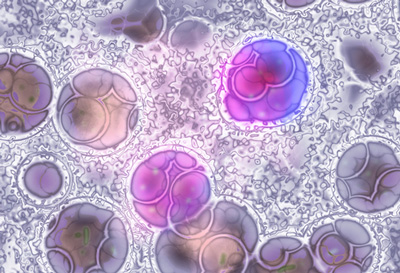
Acute myeloid leukaemia cells matured into dendritic cells and then natural killer cells
A high percentage of acute myeloid leukaemia cells express the thrombopoietin (TPO) receptor, and the effective antibody was a highly potent and selective activator of this receptor on marrow cells. When the antibody was applied to healthy immature marrow cells, it caused them to mature into blood-platelet-producing cells called megakaryocytes. However, when the antibody was applied to acute myeloid leukaemia cells, they matured into very different cells known as dendritic cells, key support cells in the immune system.
By itself, this could be a valuable therapeutic strategy, but it wasn’t the end of the story. Lerner’s team noted that, with longer exposures to the antibodies and certain other lab-dish conditions, the induced dendritic cells developed further—into cells that closely resembled natural killer (NK) cells.
NK cells can be effective against viruses and bacteria—and cancer cells—even without prior exposure. They don’t have highly specific receptors for recognising individual targets, as T-cells do, but instead are capable of detecting, in a general way, when a nearby cell is infected or cancerous.
“That antibody could have turned those acute myeloid leukaemia cells into a lot of other cell types, but somehow we were lucky enough to get NK cells,” Lerner said.
The team examined these induced NK cells with electron microscopy and observed that many of the cells had extended tendrils through the outer membranes of neighbouring leukaemic cells—their erstwhile brethren. In lab dish tests, a modest number of these NK cells wiped out about 15% of the surrounding acute myeloid leukaemia cell population in just 24 hours.
Fratricidal therapies
Curiously, the induced NK cells’ cancer-killing effect appeared to be purely fratricidal. The researchers found that unrelated breast cancer cells did not die off in large numbers when in the presence of the NK cells.
Why the induced NK cells appear to target only closely related cells isn’t yet clear. In principle, though, there are yet-to-be-discovered antibodies that would turn other cancerous cell types into fratricidal NK cells, by activating other receptors expressed on those cells.
Such fratricidal therapies, which Lerner terms “fratricidins,” would have several potential advantages. First, especially if they are antibodies, they could be clinically useful with little or no further modification. Second, their high specificity for their target receptors, and the resulting NK cells’ specificity for related cancer cells, should reduce the likelihood of adverse side effects, possibly making them much more tolerable than traditional cancer chemotherapies.
Finally, the peculiar dynamics of fratricidin therapy, in which every cancerous cell is potentially convertible to a cancer-killing NK cell, suggests that—if the strategy works—it might not just reduce the targeted cancer-cell population in a patient, but eliminate it altogether.
“We’re in discussions with pharmaceutical companies to take this straight into humans after the appropriate preclinical toxicity studies,” he said.
Related topics
Antibody Discovery
Related conditions
Breast cancer, Leukaemia
Related organisations
Cancer Research, The Scripps Research Institute (TSRI)