SARS-CoV-2-targeting antibodies persist for at least three months in COVID-19 patients
Posted: 9 October 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Two separate studies show that IgG serotype antibodies targeting the SARS-CoV-2 spike protein are still detectable in patient’s blood and saliva after 90 days.
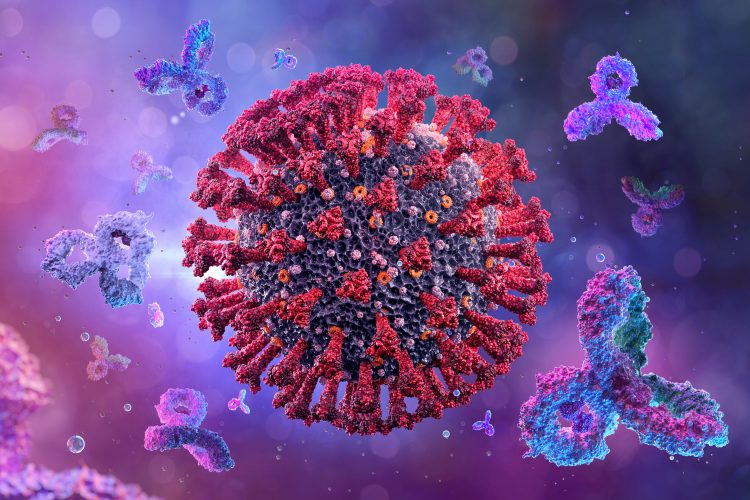
Researchers have documented the persistence of anti-SARS-CoV-2 antibodies in the blood and saliva of COVID-19 patients at least 3 months after symptom onset. In two separate studies, scientists found that the IgG serotype of antibodies are the longest-lasting antibodies and therefore could be promising targets to detect and evaluate immune responses against the virus.
They also suggest that saliva could be used as an alternative biofluid for COVID-19 antibody testing because the SARS-CoV-2-specific IgG antibodies could be detected at similar levels in both blood and saliva.
In the first study published in Science Immunology, Anita Iyer and colleagues measured anti-SARS-CoV-2 antibody responses in the blood of 343 patients with COVID-19 for up to 122 days after symptom onset. They compared these responses to those of 1,548 control individuals sampled before the pandemic. The team focused on antibodies specific to the SARS-CoV-2 spike (S) protein’s receptor binding domain (RBD).
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
To provide a baseline, the researchers estimated sensitivities of IgG, IgA and IgM antibody types at 95, 90 and 81 percent, respectively, for detecting infected individuals between 15 to 28 weeks after symptom onset. In the study they found that the S protein-specific IgM and IgA serotypes were short-lived, dropping beneath detection levels at around 49 and 71 days (respectively) after the appearance of symptoms. The S protein-specific IgG responses on the other hand, decayed slowly over a period of 90 days, with only 3 individuals losing them within this timeframe.
The authors highlighted that the levels of S-specific IgG strongly correlated with levels of neutralising antibodies in the patients and that there was no observed cross-reactivity between any SARS-CoV-2-targeting antibodies with other “common cold” coronaviruses.
Similarly the authors of the second study, Baweleta Isho and colleagues, found that while IgA and IgM antibodies targeting the RBD rapidly decayed, RBD-targeting IgG antibodies remained relatively stable for up to 105 days after symptom onset in the 402 patients they followed with COVID-19.
In this paper the researchers detected S protein-specific antibodies in both the saliva and the blood of the patients. Charting the patients’ antibody responses from 3 to 115 days after symptom onset and comparing these profiles to 339 pre-pandemic controls, the team found that COVID-19 patients had peak IgG levels at 16 to 30 days after the appearance of symptoms. Levels of all S-specific IgG, IgM and IgA antibodies in the blood positively correlated with levels observed in matched saliva samples.
“Given that the virus can also be measured in saliva by PCR, using saliva as a biofluid for both virus and antibody measurements may have some diagnostic value,” concluded the authors of the second study, also published in Science Immunology.
Related topics
Antibodies, Disease Research, Immunology
Related conditions
Coronavirus, Covid-19
Related people
Anita Iyer, Baweleta Isho