Lymphatic endothelial cells are found to promote the spread of melanoma
Posted: 4 May 2018 | Drug Target Review | No comments yet
Scientists have investigated the mechanisms by which the lymphatic endothelial cells modulate metastasis in melanoma, providing new targets for therapy development.
Despite the declining death rates for many individual cancer types, mortality for a few cancers has stabilised or even increased. One of these is melanoma owing to its ability, in later stages, to spread to other parts of the body. Melanoma is considered metastatic – termed Stage IV melanoma – when the cancer cells have spread through the lymph nodes to distant sites in the body, most often affecting the liver, lungs, bones and brain.
Primary melanomas usually grow and spread horizontally on the surface of the skin before penetrating into deeper layers of the dermis where they can reach the lymph and blood vessels. Lymphatic invasion and lymph node metastasis correlate with poor clinical outcomes for melanoma patients. In addition to providing a direct route for dissemination, the lymph vessels have been proposed to directly modulate the metastatic process through mechanisms that have remained elusive.
Commenting on the precise focus of their study into the lymphatic system, Professor Päivi Ojala from the University of Helsinki, explains: “Because the mechanisms and functional contribution of lymphatic dissemination in distant organ melanoma metastasis remain incompletely understood, we have investigated the contribution of the cells that form the walls of the lymphatic vessels, the lymphatic endothelial cells, to human melanoma cell invasion and metastasis”.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
“In particular, our goal was to uncover the critical factors in the tumour lymphatic microenvironment that promote the melanoma cell distant organ metastasis and thereby generate new leads and potential targets (for) more efficient treatments and prognosis for metastatic cancer.”
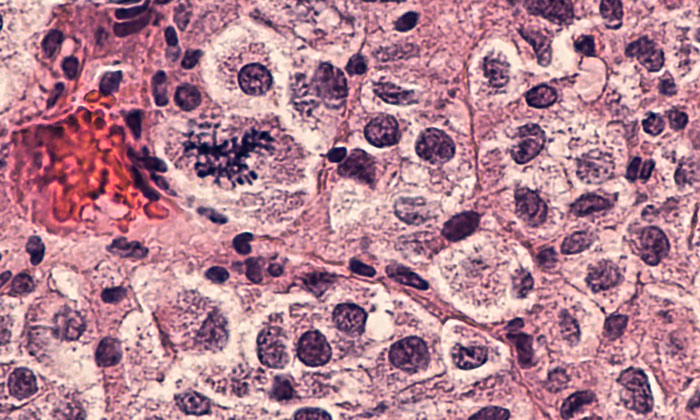
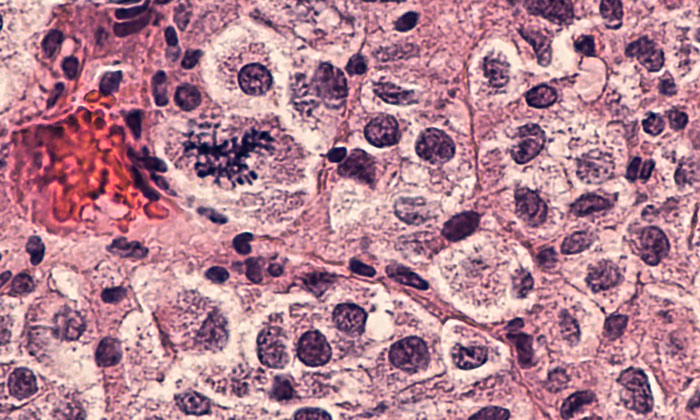
Growing human melanoma cells in co-cultures with human primary lymphatic endothelial cells increased the invasive growth of melanoma cells in cell culture conditions that mimick the tissue environment. This facilitated melanoma distant organ metastasis in mice implanted with human melanoma cells. This lymphatic endothelium-mediated change in the melanoma was dependent on MMP14, Notch3 and b1-integrin proteins, and MMP14 and Notch3 were necessary for the increased metastasis of human melanoma cells in a zebrafish tumour model.
The study uncovers a unique mechanism whereby direct contact with lymphatic endothelial cells promotes melanoma metastasis.
“These findings can represent new leads that clinicians can consider as prognostic markers for metastasis and the pharmaceutical industry can pursue for further therapeutics development,” Professor Ojala said.
Related topics
Disease Research, Drug Leads, Oncology
Related conditions
Metastatic melanoma
Related organisations
University of Helsinki
Related people
Prof Päivi Ojala