A new machine learning tool identifies drugs to minimise fibrosis
Posted: 5 February 2024 | Drug Target Review | No comments yet
The computer model enables a better understanding of how drugs affect fibroblasts and finds a promising candidate to prevent heart scarring.
A new approach to machine learning (ML) has been developed by researchers from the University of Virginia (UVA) to identify drugs that help minimise dangerous scarring following a heart attack or other injuries. Already, the tool has found a promising candidate to help prevent heart scarring in a different way to previous drugs. The scientists state that their model could predict and explain the effects of drugs for other diseases as well.
Dr Anders Nelson, a computational biologist and former student in the lab of UVA’s Dr Jeffrey Saucerman, commented: “Many common diseases such as heart disease, metabolic disease and cancer are complex and hard to treat…Machine learning helps us reduce this complexity, identify the most important factors that contribute to disease and better understand how drugs can modify diseased cells.”
Dr Saucerman, at UVA’s Department of Biomedical Engineering, explained: “On its own, machine learning helps us to identify cell signatures produced by drugs…Bridging machine learning with human learning helped us not only predict drugs against fibrosis but also explain how they work. This knowledge is needed to design clinical trials and identify potential side effects.”
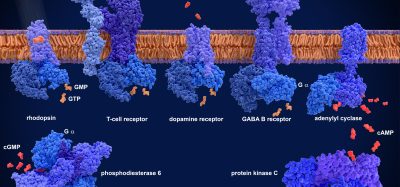
Dr Saucerman and his colleagues combined a computer model based on decades of human knowledge with machine learning to better understand how drugs affect cells named fibroblasts. Fibroblasts help repair the heart after injury by producing collagen and contracting the wound. However, they can cause harmful scarring, called fibrosis, as part of this process.
The team aimed to discover a selection of promising drugs that would provide clinicians more ability to prevent scarring and therefore improve patient outcomes. Previously, attempts to find drugs targeting fibroblasts have only concentrated on certain aspects of fibroblast behaviour, and how these drugs work often remains uncertain. To overcome this, the teams’ new approach called “logic-based mechanistic machine learning” predicts drugs but also predicts how they affect fibroblast behaviours.
The effect of 13 promising drugs on human fibroblasts was observed and then that data was used to train the ML model. The model predicted a new explanation of how the drug pirfenidone, already approved by the federal Food and Drug Administration (FDA) for idiopathic pulmonary fibrosis, suppresses contractile fibres inside the fibroblast that stiffen the heart. Also, the model predicted how another type of contractile fibre could be targeted by the experimental Src inhibitor WH4023, which they experimentally validated with human cardiac fibroblasts.
Although more research is required to verify the drugs work as intended in animal models and human patients, the UVA scientists say their research suggests mechanistic machine learning represents a significant tool for scientists seeking to discover biological cause-and-effect.
“We’re looking forward to testing whether pirfenidone and WH4023 also suppress the fibroblast contraction of scars in preclinical animal models,” Dr Saucerman concluded. “We hope this provides an example of how machine learning and human learning can work together to not only discover but also understand how new drugs work.”
This study was published in the Proceedings of the National Academy of Sciences (PNAS).
Related topics
Drug Discovery, Machine learning
Related conditions
fibrosis, Heart attack
Related organisations
University of Virginia (UVA)
Related people
Dr Anders Nelson (UVA), Dr Jeffrey Saucerman (UVA)