Type 1 regulatory cells limit immunotherapy success
Posted: 8 August 2024 | Drug Target Review | No comments yet
Scientists discovered the number of Tr1 cells increased as tumours grew larger, making mice insensitive to immunotherapy.
Scientists at Washington University School of Medicine discovered that type 1 regulatory (Tr1) cells inadvertently limit immunotherapy’s potency against sarcoma tumours in mice models.
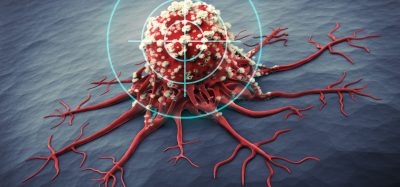
Despite immunotherapy’s successes, only around one in five people respond favourably to it, so the team aimed to address its weaknesses. Dr Robert Schreiber, the Andrew M. and Jane M. Bursky Distinguished Professor in the Department of Pathology & Immunology, and director of the Bursky Center for Human Immunology & Immunotherapy at Washington University School of Medicine, was senior leader of the study. He explained: “By removing or circumventing that barrier in mice, we successfully reenergised the immune system’s cancer-fighting cells and uncovered an opportunity to expand the benefits of immunotherapy for more cancer patients.”
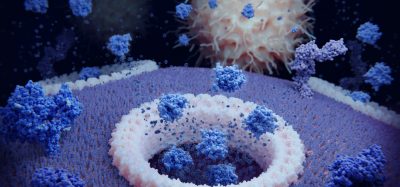
Cancer vaccines, which target mutant proteins specific to the patient’s tumour, offer a novel approach to personalise cancer immunotherapy. They induce killer T cells to combat tumour cells while leaving healthy cells unharmed. Previously, Dr Schreiber’s group demonstrated that effective vaccines also activate helper T cells.
However, in the latest study, when they added larger amounts of the helper T cell target to supercharge the vaccine, they generated a different type of T cell that restrained tumour rejection. Dr Hussein Sultan, an instructor in pathology and immunology, and first author of the study, commented: “We thought that more helper T cell activation would optimise elimination of the sarcoma tumours in mice…Instead, we found that vaccines containing high doses of helper T cell targets induced inhibitory Tr1 cells that completely blocked tumour elimination. We know that Tr1 cells normally control an overactive immune system, but this is the first time they have been shown to dampen its fight against cancer.”
The team studied previously published data and discovered that tumours from patients who responded poorly to immunotherapy had more Tr1 cells compared with tumours of patients who had responded well. Furthermore, in mice, the number of Tr1 cells increased as tumours grew larger, making the mice insensitive to immunotherapy.
Asher Biotherapeutics, of which Dr Schrieber is a co-founder, developed a drug which was provided to the researchers. With modifications in the interleukin 2 (IL-2) protein, it enhances killer T cells and reduces the toxicity of unmodified IL-2 treatments. The team treated the vaccinated mice with this to bypass the inhibiting cells.
Dr Schrieber is indirectly involved in Asher Biotherapeutics’ clinical trials testing the human version of the drug as a monotherapy in cancer patients. If successful, the drug has the potential to be assessed in combination with cancer treatment vaccines.
This study was published in Nature.
Related topics
Cancer research, Clinical Trials, Drug Development, Immunotherapy, Oncology, T cells
Related conditions
Cancer Research, sarcoma
Related organisations
Asher Biotherapeutics, Washington University School of Medicine