Bacterial pathogens found in brains of Alzheimer’s patients
Posted: 24 January 2019 | Drug Target Review | No comments yet
Researchers have found bacterial pathogens in the brains of Alzheimer’s patients, and have shown that they could be driving progression of the disease…


A bacterium, Porphyromonas gingivalis, ordinarily associated with chronic gum disease, has been shown to drive Alzheimer’s disease pathoglogy.
Researchers at the University of Louisville detailed in their study how P. gingivalis was observed, with Dr Jan Potempa at the Department of Oral Immunology and Infectious Diseases in the School of Dentistry part of the study.
According to Dr Potempa, although infectious agents have been implicated in the development and progression of Alzheimer’s disease, the evidence of causation has not been convincing.
However, “we now have strong evidence connecting P. gingivalis and Alzheimer’s pathogenesis, but more research needs to be done before P. gingivalis is explicitly implicated in the causation or morbidity of Alzheimer’s disease.
“An even more notable aspect of this study is demonstration of the potential for a class of molecule therapies targeting major virulence factors to change the trajectory of Alzheimer’s disease, which seems to be epidemiologically and clinically associated with periodontitis,” Dr Potempa said.
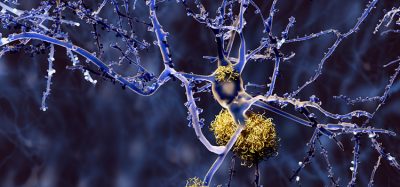
In animal models, oral P. gingivalis infection led to brain colonisation and increased production of amyloid beta (Aβ), a component of the amyloid plaques commonly associated with Alzheimer’s disease.
The study team also found the organism’s toxic enzymes, or gingipains, in the neurons of patients with Alzheimer’s disease. Gingipains are secreted and transported to outer bacterial membrane surfaces and have been shown to mediate the toxicity of P. gingivalis in a variety of cells. The team correlated the gingipain levels with pathology related to two markers: tau, a protein needed for normal neuronal function, and ubiquitin, a small protein tag that marks damaged proteins.
Seeking to block P. gingivalis-driven neurotoxicity, Cortexyme set out to design a series of small molecule therapies targeting P. gingivalis gingipains. In preclinical experiments detailed in the paper, researchers demonstrated that by inhibiting the compound COR388, there was reduced bacterial load of an established P. gingivalis brain infection, blocked Aβ42 production, reduced neuroinflammation and protected neurons in the hippocampus – the part of the brain that mediates memory and frequently atrophies early in the development of Alzheimer’s disease.
In October 2018, Cortexyme announced results from its Phase 1b clinical trial of COR388 at the 11th Clinical Trials in Alzheimer’s Disease Conference. COR388 showed positive trends across several cognitive tests in patients suffering from Alzheimer’s disease, and the company plans to initiate a Phase 2 and 3 clinical trial of COR388 in mild to moderate Alzheimer’s disease in 2019.
The study was published in Science Advances.
Related topics
Disease Research, Drug Discovery, Research & Development
Related conditions
Alzheimer’s disease
Related organisations
University of Louisville
Related people
Dr Jan Potempa