Siah2 protein discovered as a regulator of the immune system
Posted: 8 January 2020 | Drug Target Review | No comments yet
A new study has revealed that the Siah2 protein is crucial to control Tregs in mice, which can reduce the effectiveness of immunotherapies.
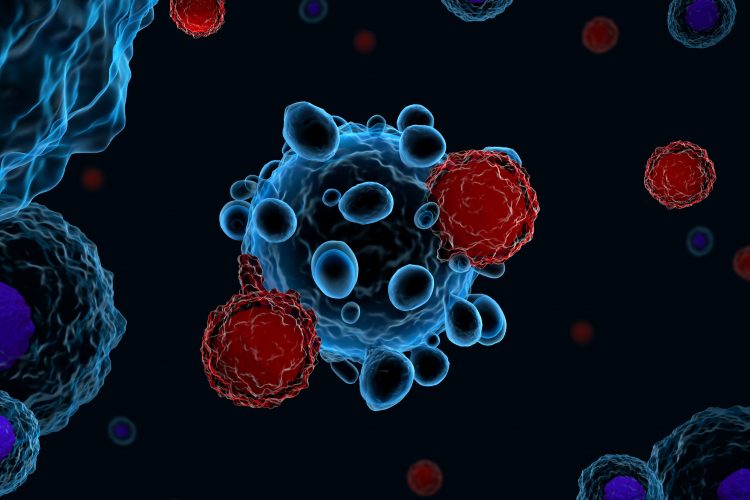
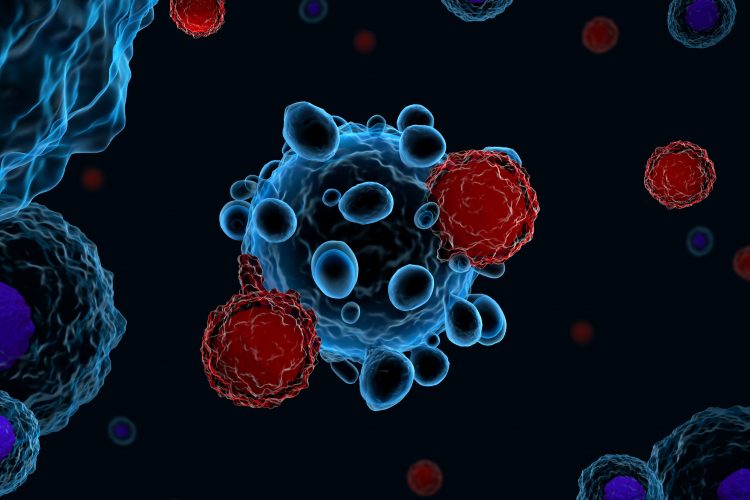
Researchers have identified a new technique to improve the immune system‘s ability to fight cancer. Using mouse models they demonstrated that the Siah2 protein is essential to control T regulatory cells (Tregs), which can limit the effectiveness of currently used immunotherapies.
The study was conducted at the Sanford Burnham Prebys Medical Discovery Institute, in collaboration with NYU Langone’s Perlmutter Cancer Center, both US.
“While Siah2 is involved in control of activities that govern cancer development, this study offers the first direct evidence for its role in the immune system, namely in anti-tumor immunity,” says Dr Ze’ev Ronai, professor in Sanford Burnham Prebys’ Tumor Initiation and Maintenance Program and senior author of the study. “Our study shows that a PD-1 inhibitor can be used to treat tumors that currently do not respond to this therapy, when administered in mice lacking the Siah2 gene, thereby offering a means to expand the effectiveness of immunotherapy. The findings also provide further justification for our efforts to find a drug that blocks Siah2.”
In the study, the scientists used genetically engineered mice that did not produce the Siah2 protein and then introduced BRAF-mutant melanoma, a mutation that occurs in about half of human melanomas. This approach allowed the researchers to study the role of Siah2 in the tumour’s microenvironment, of which the immune system is a major component. In the absence of the Siah2 gene, the melanoma tumors receded, which contrasted to mice with the Siah2 gene, in which the tumour continued to grow. Giving these mice anti-PD-1 therapy effectively eliminated melanoma that otherwise resisted this therapy, demonstrating a new path to enhance the effectiveness of current immunotherapies.
The scientists discovered that in the Siah2 mutant mice, the tumours were infiltrated by killer but not Treg immune cells, indicating the immune system was more active in clearing the tumours. The lack of the Treg cells was attributed to reduced proliferation and recruitment into the tumour due to the role of Siah2 and its control of cell cycle regulatory proteins.
Ronai explains: “In our study, mice lacking the Siah2 gene were able to mount an immune attack against melanoma. Moreover, the effectiveness of Siah2 in immunotherapy was demonstrated for ‘cold’ tumors – those that do not respond to immunotherapy – which were effectively eliminated by a PD-1 blockade in Siah2-mutant mice.”
The researchers say that their findings offer a new means to make immunotherapies more effective in individuals who do not respond to anti-PD-1 therapy.
The findings were published in Nature Communications.
Related topics
Disease Research, Drug Targets, Immuno-oncology, Immunotherapy, Oncology
Related conditions
Cancer
Related organisations
NYU Langone's Perlmutter Cancer Center, Sanford Burnham Prebys Medical Discovery Institute
Related people
Dr Ze'ev Ronai