T-cell exhaustion may limit long-term immunity in COVID-19 patients
Posted: 22 January 2021 | Hannah Balfour (Drug Target Review) | No comments yet
Researchers suggest patients who develop mild COVID-19 may not be able to fight reinfection very effectively because their CD8+ T cells show signs of exhaustion.
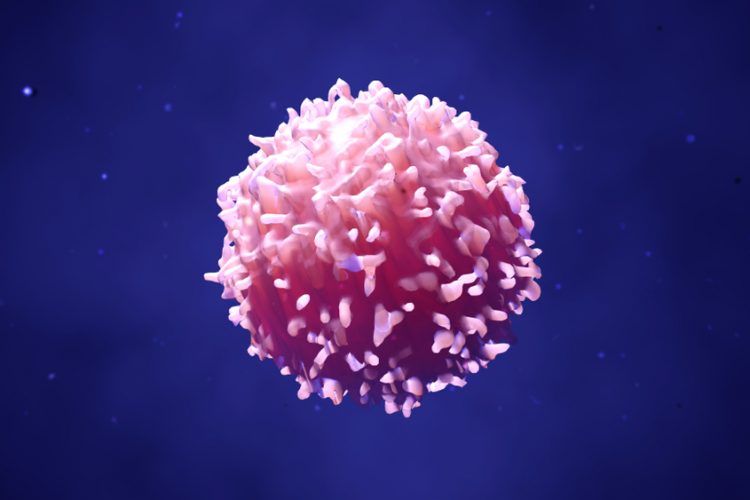
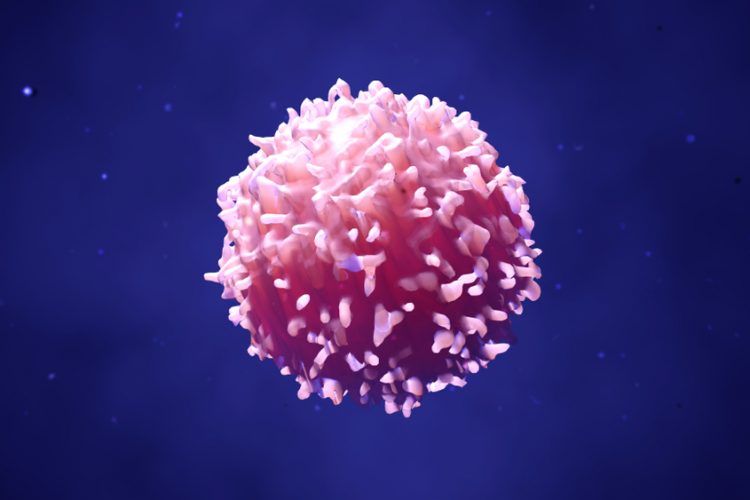
New data suggests people who develop severe COVID-19 symptoms may be better protected from reinfection. According to the investigators, the memory T cells of people who experience mild COVID-19 symptoms show the molecular signs of exhaustion and therefore could have a reduced ability to fight reinfection.
In a new study, researchers from the US’s La Jolla Institute for Immunology (LJI) and the UK’s University of Liverpool and University of Southampton used single-cell transcriptomics to study gene expression in more than 80,000 CD8+ T cells isolated from both COVID-19 patients and non-exposed donors. CD8+ T cells destroy virus-infected host cells and a subset, called memory CD8+ T cells, remain after the primary infection is cleared to help protect against reinfection.
Overall, they examined the CD8+ T cells from 39 COVID-19 patients and 10 subjects who had never been exposed to the virus (their blood samples were given before the pandemic). Of the COVID-19 patients, 17 patients had a milder case that did not require hospitalisation, 13 had been hospitalised, and nine had needed additional intensive care unit (ICU) support.
The researchers said they were surprised to find that patients with milder COVID-19 cases had weaker CD8+ T-cell responses and those who were severely ill (requiring hospitalisation or ICU support) had the strongest CD8+ T-cell responses.
The team had expected to find the opposite, that those with milder cases had the strongest responses, as they fought off the infection best. But the scientists found that in these patients, CD8+ T cells showed the molecular signs of a phenomenon called T-cell exhaustion, where the cells receive so much immune system stimulation during a viral attack that they are less effective in doing their jobs.
While more research is needed, the study leaders LJI Professor Dr Pandurangan Vijayanand and Christian Ottensmeier, MD, PhD, FRCP, a professor at the University of Liverpool and adjunct professor at LJI, said they believe it is worth studying whether T-cell exhaustion in the mild COVID-19 cases may hinder a person’s ability to build long-term immunity.
“People who have severe disease are likely to end up with a good number of memory cells,” said Vijayanand. “People with milder disease have memory cells, but they seem exhausted and dysfunctional – so they might not be effective for long enough.”
According to the investigators, the study provides a valuable window into CD8+ T-cell responses but is limited because it relies on the CD8+ T cells found in blood samples. They now intend to shed light on how T cells within the tissues hit hardest by SARS-CoV-2, such as the lungs, react to the virus. The scientists said this is important because the memory T cells in these tissues will be doing most of the work to provide long-term immunity.
“This study is very much a first step in understanding the spectrum of immune responses against infectious agents,” said Ottensmeier. Going forward, the researchers also hope to use single-cell sequencing techniques to look at CD8+ T cells in cancer patients with COVID-19 infection.
The study was published in Science Immunology.
Related topics
Disease Research, Immunology, In Vitro, Sequencing, T cells
Related conditions
Coronavirus, Covid-19, viral infections
Related organisations
La Jolla Institute for Immunology (LJI), Southampton University, the University of Liverpool