‘Delete-to-recruit’: new gene-editing method targets sickle cell
Posted: 25 June 2025 | Drug Target Review | No comments yet
Researchers have developed a novel gene therapy approach that reactivates dormant genes by repositioning them closer to genetic switches called enhancers – showing promise for treating blood disorders like sickle cell disease.
In a new advancement for gene therapy, researchers from the Hubrecht Institute (De Laat group), Erasmus MC, and Sanquin have developed a new method that can reactivate dormant genes by altering their proximity to powerful genetic switches – called enhancers. Their approach, dubbed ‘delete-to-recruit’, uses CRISPR-Cas9 to remove the DNA segment separating a gene from its enhancer – reviving gene activity without introducing any foreign genetic material.
The findings, published in the journal Blood, demonstrate the technique’s potential to treat genetic diseases by restoring function to genes that are otherwise inactive in adulthood.
How enhancers control gene activity
Genes carry the instructions for producing proteins – the essential workers of our cells. However, not all genes are switched on at the same time. Many genes are tightly regulated, turning on only during specific life stages or under certain conditions. Enhancers, which act like genetic switches, help control this regulation by turning genes on and off.
“Enhancers can be located next to the gene they control, but can also be far away on the DNA,” explained Anna-Karina Felder, one of the study’s first authors. “In this study, we discovered that it’s possible to activate a gene by bringing it closer to an enhancer.”
CRISPR: cutting the distance
To manipulate the distance between a gene and its enhancer, the team used CRISPR-Cas9, a molecular tool that acts like highly precise genetic scissors.
“We directed the scissors to cut out a piece of DNA between an enhancer and its gene, bringing them closer together,” said Felder. “In adult cells, this successfully reactivated genes that are normally only active during embryonic development.” The researchers call this approach ‘delete-to-recruit’, describing it as a completely new way to turn on dormant genes.
Treating sickle cell disease and beta-thalassemia
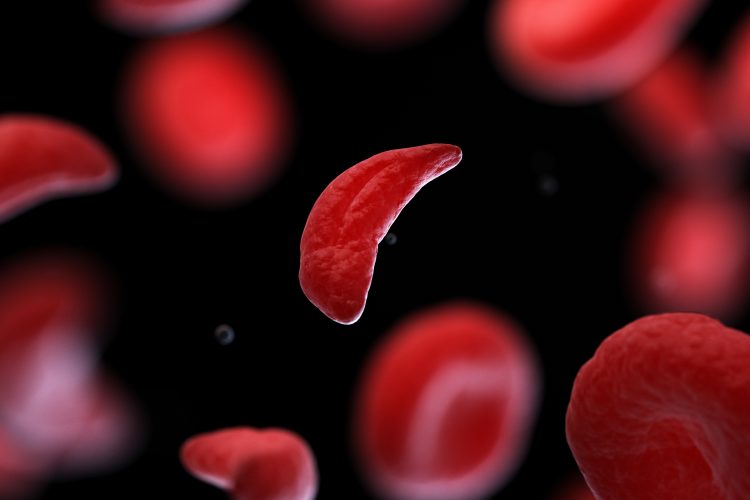
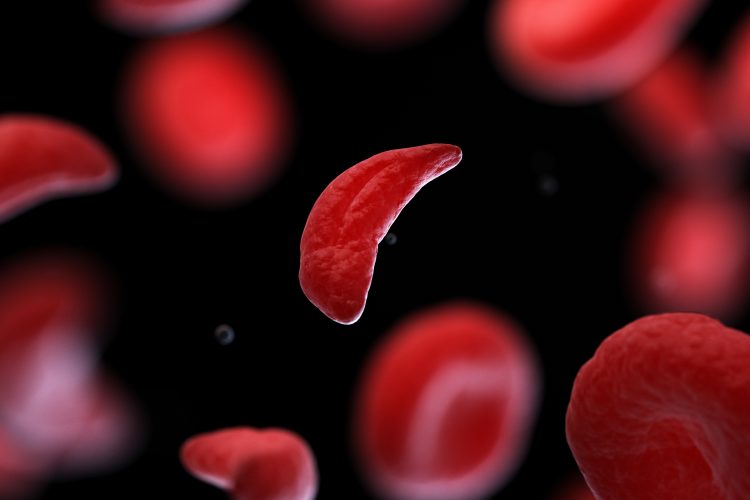
The team focused their study on two inherited blood disorders – sickle cell disease and beta-thalassemia. Both conditions are caused by faults in the adult globin gene, which is responsible for producing haemoglobin. The faulty gene results in malformed red blood cells that break down prematurely, causing chronic anaemia, fatigue and long-term organ damage.
In these cases, the foetal version of the globin gene could provide a workaround.
“In people with sickle cell disease or beta-thalassemia, it’s the adult globin gene – the main engine that powers red blood cells – that is broken. But foetal globin is like a backup engine,” said Felder. “By switching it back on, we can repower the red blood cells and possibly cure these patients.”
Validated in human blood stem cells
The researchers collaborated with Erasmus MC (Philipsen group) and Sanquin (Van den Akker group) to test the method in both healthy donor cells and cells from patients with sickle cell disease. They confirmed that the technique worked in blood stem cells, which are responsible for generating all types of blood cells, including red blood cells.
By reactivating foetal globin in these stem cells, the therapy could potentially generate a continuous supply of healthy red blood cells in patients, offering a long-lasting solution to their condition.
A broader impact for gene therapy
While the research is still in its early phases, its implications are vast.
While we’re still in the early stages, this research lays important groundwork for the development of new gene therapies
“While we’re still in the early stages, this research lays important groundwork for the development of new gene therapies,” said Felder. She added that the technique could extend beyond blood diseases to any condition where reactivating a ‘backup’ gene could compensate for a malfunctioning one.
“Editing the distance to an enhancer, instead of the genes themselves, could offer a versatile therapeutic approach,” she concluded.
A potentially safer, more accessible alternative
Although a gene therapy for sickle cell disease was approved in Europe in 2024, its high cost and complex mechanism limit its use. That treatment involves editing a repressor gene to reactivate foetal globin, but it may also affect other genes in unpredictable ways.
The delete-to-recruit method could offer a safer and more cost-effective alternative. By repositioning DNA without adding or altering genes – it may reduce risks and increase accessibility for patients around the world.
Related topics
Clinical Trials, CRISPR, Drug Discovery Processes, Epigenetics, Gene Therapy, Genetic Analysis, Genome Editing, Molecular Biology, Molecular Targets, Precision Medicine, Translational Science
Related organisations
Erasmus MC, Hubrecht Institute (De Laat group), Sanquin
Related people
Anna-Karina Felder (P.H.D Hubrecht Institute)








