Breaking new ground in endometriosis treatment
Posted: 14 November 2023 | Hugo Vankelecom (KU Leuven) | No comments yet
Endometriosis is a debilitating condition that affects millions of women worldwide, causing chronic pain, infertility, and a host of other distressing symptoms. Current treatments offer limited relief, but they do not address the cause of the disease. Professor Hugo Vankelecom, at the helm of the CurE-me project, is on a mission to revolutionise endometriosis treatment. His work leverages a unique organoid biobank and the support of the BioInnovation Institute (BII) to screen for more effective, targeted therapies. In this interview, we explore the project’s goals, challenges, and the vital role the organoid biobank and BII play in advancing the fight against endometriosis.
What is the primary goal of the CurE-me project, and how does it aim to address the issue of endometriosis?
The primary goal is to find better, more efficient and more targeted therapeutics for endometriosis (hence “CurE-me” or Curing Endometriosis). Currently, there are no satisfactory or curative treatments available. Treatment is usually directed toward symptom control and pain relief (eg, using hormones and painkillers) and/or is invasive (ie, surgical removal of the endometriotic lesions). The current therapies fail to reverse or cure the disease since they do not address its root cause, i.e. the growth and thriving of ectopic lesions that underlie the disease burden (see below). At present, there are no drugs that directly target these ectopic endometrial tissue (out)growths.
In recent years, our research group has developed a unique 3D organoid model that closely recapitulates human endometrial tissue –healthy or diseased (such as endometriotic lesions). In CurE-me, we will screen many drugs for effects on these endometriotic organoids, to find new and more targeted medicines for endometriosis.
Can you explain the significance of the organoid biobank developed by Vankelecom’s research group and how it will be utilised in the hunt for endometriosis treatments?
Through close collaboration with the endometriosis gynaecologists in University Hospitals (UZ) Leuven, we receive(d) many biopsies from patients with endometriosis. These biopsies cover all types (superficial, deep infiltrating and cystic ovarian endometriosis (endometrioma)) and ASRM stages (I to IV) of endometriosis.
Our lab established (and still does) a unique biobank of organoid lines from these patients’ endometriotic lesions. The organoids closely recapitulate the disease hallmarks and are robustly expandable. We will now harness this organoid biobank into an endometriosis drug discovery platform, where we will screen multiple compound libraries. Importantly, our biobank also contains organoid lines derived from healthy endometrium, which allows us to simultaneously test for safety and toxicity of the compounds, ie, affecting the endometriotic ectopic lesions but not (or only minimally) the healthy endometrium. Together, the biobank allows us to identify non-toxic therapeutics to treat endometriosis.
What role does the BioInnovation Institute (BII) play in supporting the CurE-me project, and how does this support accelerate the project’s progress?
The BioInnovation Institute (BII) makes up to 1 million € per year available for our drug discovery process through its Bio Studio program. In addition, the BII will support us in the areas of infrastructure, access to investors and intellectual property. Patents that would arise from CurE-me remain at KU Leuven – a unique asset of the BII’s Bio Studio program. The CurE-me project will lay the foundation for a potential spin-off, which would be established after three years under the guidance of KU Leuven Research & Development (LRD), our university’s technology transfer office. LRD already supported our research into endometriosis with a Wellcome Trust-LRD Ignite Grant of €40,000. Their business developers also helped set up the process with the BII. We now very much look forward to a fruitful collaboration to find the much-needed treatment for endometriosis, to help and cure millions of women suffering from this disease.
Could you elaborate on the unique challenges Professor Hugo Vankelecom faced as a scientist in bringing potential endometriosis treatments to the market and how BII’s expertise complements his efforts?
Professor Hugo Vankelecom and his group work in the field of women’s health, and develop new research and preclinical models to study endometrial (and other) diseases. They established endometriosis research ‘avatars’ by turning endometriotic lesions into powerful and reliable organoid models. These models are currently used to decipher endometriosis pathobiology as well as to find new and better (targeted) drugs to affect the growth of these lesions. Professor Vankelecom already had the latter ambition for a long time, and his team already performed some drug screening tests although at very low scale, with upscaling being a challenge. Another challenge was (and still is) to obtain funding for this kind of projects, because of the under-funding of women’s health research in general, and endometriosis in particular, and the very low attention that has been given to the disease until very recently. Hence, BII and the granted CurE-me project will function as a very important accelerator for Vankelecom’s ambition, now finally enabling to move full force in this field.
What are the current treatment options available for endometriosis, and why is there a need for more effective treatments?
Current options include surgical (laparoscopic) removal of the endometriotic lesions and medical treatment, mainly relieving (some of) the symptoms but not curing. Surgery provides relief to women with endometriosis-associated pain but symptoms recur in up to 75 percent of the cases within 2 years. The mainstay of medical management is ovarian suppression and includes treating patients with the oral contraceptive pill, progestins or gonadotropin-releasing hormone agonists or antagonists. However, progestins and gonadotropin-releasing hormone agonists are often only useful for limited periods due to their undesirable side effects, necessitating change or use of additional medication. These hormonal therapies are also not compatible with a desire to become pregnant. Besides hormonal therapies, pain medication including nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, is used. It is clear that current treatments may help and relieve some symptoms, but are not highly effective, meaning that patients keep suffering from the burdening disease in a chronic manner.
How does the presence of endometriotic lesions impact the lives of women suffering from endometriosis, and what are the potential long-term consequences of the disease?
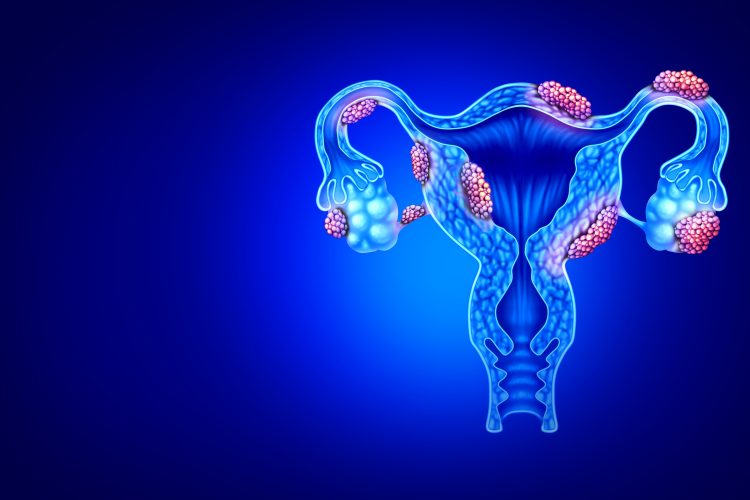
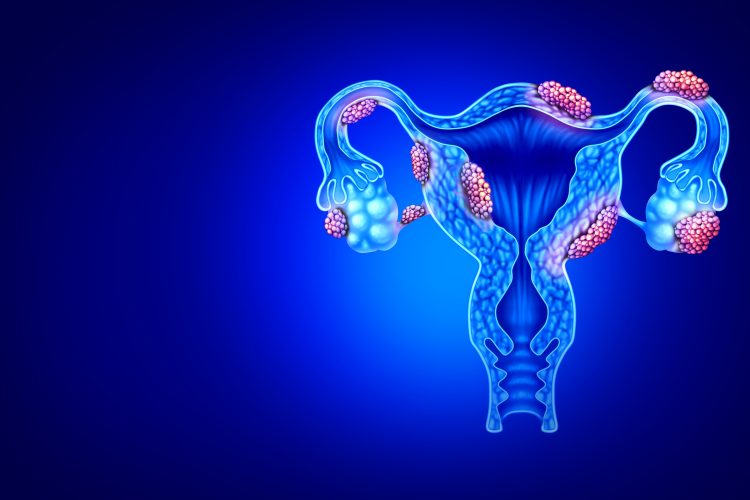
Endometriosis is a chronic disease that affects an estimated 1 in 10 women of childbearing-age worldwide, meaning a total of 190 million. In these patients, cells from the womb’s inner lining (i.e. endometrium), which normally occur on the inside of the uterus, also grow outside the uterus where they form serious lesions. In many patients, these ectopic outgrowths lead to severe pain (especially during menstruation) that is very exhausting. Many additional complaints occur, such as heavy or irregular periods, pain during or after sex, and fatigue or low energy, all also often leading to mental problems (such as depression). Moreover, endometriosis is one of the most common conditions linked to female infertility. The American Society for Reproductive Medicine (ASRM) reports that 25-50% of women with infertility have endometriosis. It is currently not really known how endometriosis causes infertility.
What role does the peritoneum play in endometriosis, and how does tissue growth in this area contribute to the disease’s symptoms and complications?
Endometriosis is defined by the presence of endometrial(like) tissue outside the uterus, most commonly attached to the pelvic peritoneum. Superficial endometriosis, characterized by the presence of lesions on the peritoneum, is indeed the most prevalent endometriosis type, comprising around 80% of all endometriosis diagnoses. Several studies indicate that the peritoneal mesothelium, a thin layer of cells that lines the inside of the abdomen, also plays an important role in the development and progression of endometriosis.
These ectopic outgrowths in the peritoneum contribute to the disease symptoms in several ways. At menstruation, not only endometrial tissue in the womb sheds and bleeds, but also endometriotic lesions outside the uterus. The resulting irritation and inflammation cause pain. Moreover, this remodelling of the ectopic lesions may cause abdominal organs to adhere to each other, causing further pain and organ/body dysfunctions. Scar tissue can also develop from the endometriotic lesions and contribute to pain. Thus, the pelvic anatomy becomes distorted, with pelvic adhesions which also lead to deficient fertility via mechanical disruptions, together with negative effects on oocytes, embryos, fallopian tubes and embryo transport.
About the author


Lab Director of the Stem Cell and Developmental Biology Unit at KU Leuven
Hugo Vankelecom is a Professor and Lab Director of the Stem Cell and Developmental Biology unit at KU Leuven. His research group investigates the role of stem cells in tissues in both health and disease primarily focusing on organs involved in endocrinology and reproduction, in particular the pituitary gland, the master regulator of our hormonal system, and the uterus and ovary, critical organs for successful pregnancy and procreation.
Related conditions
endometriosis
Related organisations
KU Leuven
Related people
Hugo Vankelecom (KU Leuven)








