Transforming cancer treatment for greatest impact
Posted: 15 January 2024 | Dr Lev Becker (Onchilles Pharma) | No comments yet
In this Q&A, Dr Lev Becker, Associate Professor, University of Chicago and Cofounder of Onchilles Pharma, reveals how his company is directing research into neutrophil biology to the advantage of cancer patients that need it most.
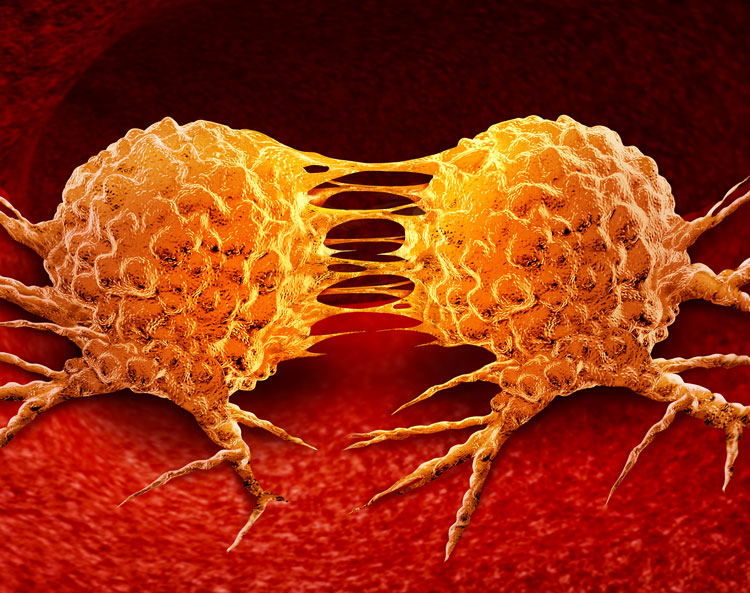
Cancer is a disease driven by variable genetic mutations. Overcoming this variability while sparing normal cells has stymied broad-acting therapeutic development. Our innate immune system evolved to clear genetically diverse pathogens and limit host toxicity, raising the possibility that it can produce similar effects in cancer. Research1 has shown that neutrophil elastase selectively and potently kills cancer cells irrespective of their genetics and anatomical origin, mobilises adaptive immunity, and avoids resistance mechanisms.
Could you provide insights into the driving factors behind exploring novel treatments for cancer types? What aspects prompted this research direction?
The mechanism of action of neutrophil elastase leverages histone H1 dysregulation, a feature unique to cancer cells, to effectively regress primary tumours and trigger CD8+T cell-mediated attacks on metastases. Onchilles Pharma has translated this breakthrough research into a proprietary set of therapeutics and plans to start first-in-human clinical trials for its first programme, N17350, in 2024 in skin cancers, head and neck cancer, and triple-negative breast cancer. While our approach is not restricted to a particular cancer type, as N17350 induces cancer cell killing irrespective of the tumour’s genetic makeup or its location in the body, we chose skin cancers, head and neck cancer, and triple-negative breast cancer because a significant lack of effective treatments exists for these patients.
Typical response rates to immunotherapy are 40-60 percent in skin cancers, 20-30 percent in head and neck cancer, and only 15-20 percent in triple-negative breast cancer due to primary and acquired resistance mechanism, which highlights a critical unmet medical need for both initial and subsequent line of treatments for patients with these diseases. Additionally, in evaluating the effectiveness of our initial pipeline asset, we sought tumours suitable for intratumoural injection that present surface-accessible lesions.
Activation of the ELANE pathway appears pivotal. How does this activation align with the distinctive characteristics of the various cancers you are working with?
Our preclinical data show that histone H1 and CD95 – the key components of the ELANE pathway – are expressed across most, if not all, cancer types. Accordingly, the efficacy of N17350 is observed in a variety of tumour types, spanning different mutational status, anatomical origin and immune status. Immunohistochemistry staining of human tissue revealed that histone H1 levels are elevated in tumours versus healthy tissue and further elevated with increased malignancy in these indications. Based on this rationale we selected skin cancer, triple-negative breast cancer, and head and neck cancers as our initial indications for our Phase 1 trials.
The preclinical results demonstrated significant immune responses and tumour regression. Could you elaborate on the mechanisms by which these responses are initiated within cancer cells?
N17350 is a potent, selective agent that induces immunogenic cancer cell death while safeguarding essential immune cells such as T cells and dendritic cells. This process leads to robust cancer cell death and the release of tumour antigens, which can then be harnessed by a still fully functional immune system to trigger anti-tumour immune responses that reinforce efficacy.
The concept of the ‘abscopal effect’ in the 4T1 tumour model is intriguing. Could you provide further details on how this phenomenon could impact broader treatment outcomes?
Immunotherapy has become a cornerstone of cancer therapy and significantly improved patient outcomes
Immunotherapy has become a cornerstone of cancer therapy and significantly improved patient outcomes
The tumour regression at the metastatic site (abscopal effect) in the 4T1 tumour model is driven by CD8+ killer T cells. This induced anti-tumour immunity is also detectable by increased innate and adaptive immune cells in the tumour, spleen and blood. N17350 has induced this immune effect in every preclinical model tested, suggesting that its therapeutic efficacy involves direct cancer-cell killing, leading to vaccine-like properties. This holds the promise of treating primary tumours of patients with N17350 and triggering global tumour responses at metastatic sites that may lead to better and more durable outcomes.
Combining N17350 with checkpoint inhibitors in ‘cold’ tumour environments shows promise. Could you shed light on how this combination might reshape the immune landscape in the context of these specific cancers?
Immunotherapy has become a cornerstone of cancer therapy and significantly improved patient outcomes. However, an unmet need persists in patient populations that do not respond to these therapies where ~50-70 percent relapse or become refractory to them. The direct cancer cell killing and immune activation properties of N17350, which are observed in tumours of high and low infiltrating leukocytes, may improve the efficacy of immunotherapies and extend their utility into indications currently not receptive to their mechanism of action. We think that when combined with immunotherapies, this approach may prove more effective than chemotherapy regimens, as the latter can induce immunosuppression in patients.
The property of N17350 to evade resistance is noteworthy. Could you expand on the underlying mechanisms contributing to this trait and its potential implications for sustained treatment effectiveness?
Our mechanism of action leverages two main components, histone H1 and the death domain of CD95, that are essential for cancer cell fitness, making it challenging for cancer cells to modify these proteins. Indeed, we have shown that this killing mechanism works in more than 45 cancer cell lines, spanning 11 anatomical locations and a wide range of genetics (eg, KRAS, BRAF, PI3K, TP53, among others). Moreover, we have shown that repeated dosing with N17350 in vitro and in vivo fails to induce resistance or diminish its efficacy.
Given the unique attributes of skin cancers, head and neck cancer, and triple-negative breast cancer, how does N17350’s mechanism offer advantages over conventional treatment approaches tailored to these specific cancers?
N17350’s mechanism of action delivers three unique attributes for a cancer drug. It generates potent tumour cytotoxicity, induces productive changes in the immune compartment, and avoids resistance mechanisms. Immunotherapies and targeted therapies used in these indications can deliver one or two of these attributes, but our belief is that all three are needed to lead to global and durable tumour responses in these patients.
As we focus on the preclinical stage, could you share insights into the significance and prevalence of skin cancers, head and neck cancer, and triple-negative breast cancer as viable targets for groundbreaking therapeutic development?
Skin cancers, head and neck cancer, and triple‑negative breast cancer are among the most common types of cancers in the US with more than 80,000 deaths each year. In these indications, therapeutic options become limited once patients have exhausted earlier line treatments with immunotherapy alone or in combination with chemotherapy or targeted therapies. These later‑stage patients need novel treatment options that can treat heterogeneous and often treatment‑resistant tumours, making them ideal candidates for initial N17350 clinical trials.
Reference
1. Cui C, Chakraborty K, Tang XA, et al. Neutrophil elastase selectively kills cancer cells and attenuates tumorigenesis. Cell [Internet]. 2021 May 7;0(0). Available from: https://www.cell.com/cell/fulltext/S0092-8674(21)00495-5#%20
About the author
Dr Lev Becker, Associate Professor, University of Chicago and Cofounder, Onchilles Pharma
Dr Becker’s lab in the Ben May Department for Cancer Research combines proteomic, bioinformatic, immunologic and functional approaches to study innate immune cells in an unbiased manner across a spectrum of diseases and develops therapeutics to target them. Dr Becker cofounded Onchilles Pharma in 2017 to translate breakthrough research in neutrophil biology into an entirely new treatment paradigm with the potential for pan-cancer killing activity.
Related topics
Biotherapeutics, Cancer research, Chemotherapy, Drug Development, Immunotherapy
Related conditions
Head and Neck cancer, Skin cancer, Triple-negative breast cancer
Related organisations
Onchilles Pharma, University of Chicago