Immuno-oncology innovations redefining cancer treatment in 2024
Posted: 23 January 2024 | Dr Espen Basmo Ellingsen (University of Oslo), Taylor Mixides (Drug Target Review) | No comments yet
In this exclusive interview, Dr Espen Basmo Ellingsen, a luminary in cancer immunology, provides insights into the anticipated breakthroughs, collaborative endeavours, and personalised strategies that promise to elevate the effectiveness and durability of immuno-oncology interventions.
What innovative approaches and technologies are anticipated to reshape immuno-oncology treatments in 2024?
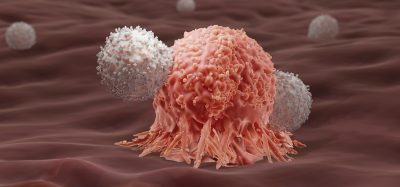
Immuno-oncology, notably through checkpoint inhibitors, has significantly reshaped cancer treatment over the past decade. The current shift focuses on enhancing their efficacy by addressing the crucial need for robust T cell responses, an apparent bottleneck for broader impact. Vaccinations against tumour antigens that are shared between tumours, or tumour antigens that arise from mutations unique to individual tumours, represent promising strategies. In April 2023, we saw the first randomised data applying an individualised vaccine in combination with checkpoint inhibition for resectable melanoma, demonstrating benefit in terms of time to disease recurrence. Cell-based therapies, such as tumour-infiltrating lymphocyte (TIL) therapy, have also drawn significant attention following promising results in a melanoma trial. In addition, 2023 brought new approvals for bi-specific T cell engagers, demonstrating impressive responses in haematological cancers, fuelling interest in this way of activating T cells to kill cancer cells. We anticipate this area to grow, especially cancer vaccines, with important read-outs expected across various cancer types in 2024.
In the evolving landscape of cancer immunotherapy, what strides are being made towards developing personalised and targeted therapies to enhance the effectiveness of immuno-oncology treatments?
Individualised cancer vaccines are tailored to each patient’s tumour, helping the immune system mount cancer-specific immune responses that can boost checkpoint inhibitor efficacy. Such approaches apply artificial intelligence (AI) and machine learning (ML) to predict mutations most likely to be good targets for the immune system. Generative AI, in general, is expected to accelerate the identification of novel tumour targets as well as compounds that can be used to disrupt tumour growth. However, while these personalised approaches are gaining increasing attention, challenges in scalability remain a significant hurdle for broader accessibility. The limitation to scaling individualised cancer vaccines underscores the opportunities for ‘off-the-shelf’ vaccines that target shared tumour antigens, such as telomerase, HPV, NY-ESO-1, and MAGE.
As we progress into 2024, how are researchers addressing challenges related to the durability of immunotherapy responses and potential resistance mechanisms, paving the way for more sustained benefits for cancer patients?
Researchers have been characterising the tumour immune microenvironment (TIME) to better understand anti-cancer immunity and resistance to immunotherapy. Building on such in-depth studies, we see novel treatment combinations being evaluated that aim to modulate the TIME to facilitate a sustained immune attack. Key targets that prevent robust and durable immune responses appear to be myeloid cells and regulatory T cells, which shape an immunosuppressive TIME. Overcoming tumour immunosuppression will be important to make immunotherapy effective in more patients and support long-term immunity against the tumour. The cancer cells can also sometimes adapt to an ongoing immune response by shutting down important targets for the immune system, so-called adaptive resistance mechanisms. Finding ways to target the tumour by circumventing these identified resistance mechanisms will be important strategies for making immunotherapy responses more long-lived.
As biomarker discovery advances, what breakthroughs are anticipated to enhance the identification of entities likely to respond positively to specific immuno-oncology interventions?
Increasing use of tumour genomic profiling is poised to improve patient selection for immunotherapies. This shift from traditional histology-based treatment decisions enables more precise therapeutic strategies based on the unique genetic makeup of the tumour rather than the tumour type. The advent of liquid biopsies offers a less invasive approach to selecting eligible patients and monitoring tumour response and resistance over time, potentially enabling timely adjustments in treatment strategies to counteract resistance mechanisms and optimise therapeutic outcomes.
How does the synergy among academic institutions, industry players, and regulatory bodies influence the trajectory of preclinical immuno-oncology research?
The trajectory of preclinical immuno-oncology research is significantly influenced by the collaborative synergy between academic institutions, industry stakeholders, and regulatory bodies. There is a lot of great science and innovation coming from academic institutions, and environments that nurture start-ups and partnerships between small biotech’s and pharmaceutical giants are pivotal for transitioning research breakthroughs into clinical applications. In regions like Norway, there’s an increasing recognition and investment in fostering such collaborative ecosystems, vital for propelling the field of immuno-oncology forward.
About the author
 Dr Espen Basmo Ellingsen
Dr Espen Basmo Ellingsen
University of Oslo
Dr Ellingsen is a Medical Doctor and holds a PhD in cancer immunology from the University of Oslo. Background in translational research from the Institute for Cancer Research at Oslo University Hospital, focusing on therapeutic cancer vaccination, induced immune responses, and their impact on the tumor microenvironment. Espen integrates clinical and research expertise as Director of Medical Affairs.
Related topics
Cancer research, Immuno-oncology
Related conditions
Cancer
Related organisations
University of Oslo