The advancement of drug-free immunotherapy
Posted: 20 March 2024 | Ellen Capon (Drug Target Review) | No comments yet
Researchers have created a neutrophil therapy, involving micropatches that maintain the cells’ antitumour state, which could offer significant clinical and commercial value.
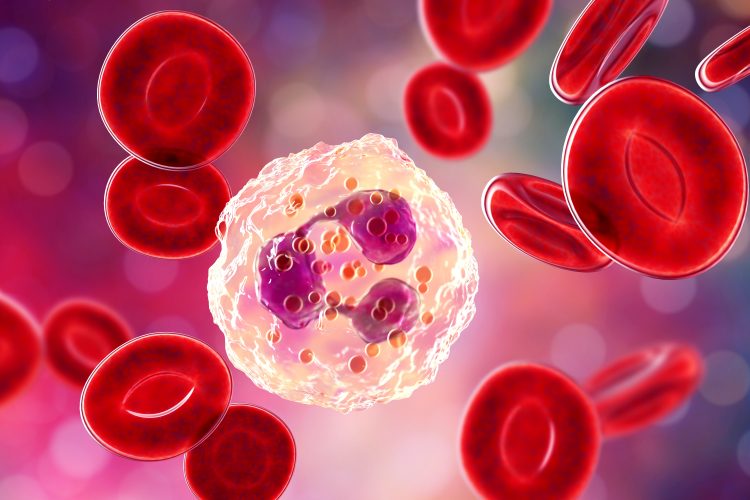
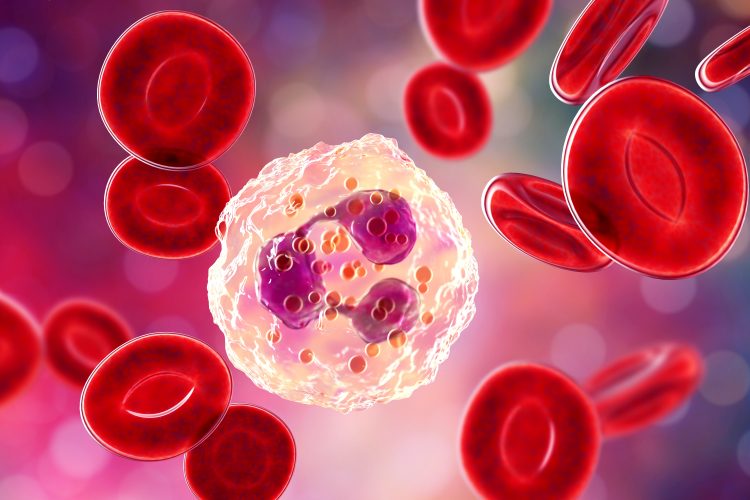
Researchers at the Wyss Institute at Harvard University and Harvard’s John A. Paulson School of Engineering and Applied Sciences (SEAS) have advanced neutrophil therapies. Neutrophils have been used for over 40 years to support the immune systems of cancer patients receiving chemotherapy, yet utilising neutrophils to directly target the cancer itself is a novel approach.
The team attached disc-shaped micropatches to neutrophils, enabling the cells to maintain their anti-tumour (N1) state, which showed promising results in mice. Terming these micropatches “backpacks”, first author Dr Ninad Kumbhojkar commented: “Unlike in previous work from our lab where we filled the backpacks with stimulatory molecules that were delivered into immune cells to activate them, we discovered that just the act of attaching empty backpacks to neutrophils is enough to activate them – making this technique attractive as a ‘drug free’ cell therapy for cancer.”
Micropatches
The most abundant circulating leukocytes in humans are neutrophils. An estimate of 107 neutrophils in mice and 1011 in humans are produced each day.1 Although they are abundant, less is known about them compared to other immune cells due to their very short life span, which averages eight hours. Despite this, recent research2 has demonstrated that neutrophils can acquire a pro-inflammatory or an anti-inflammatory state. In the context of cancer, this makes them attractive targets for immunotherapy.
Previously, backpack micropatches have been used to influence the behaviour of macrophages, successfully activating them to treat cancer, traumatic brain injury and multiple sclerosis (MS) in animal models. The scientists hypothesised that the micropatch approach could also work on neutrophils.
Neutrophils undergo a series of biological changes that signify a threat to the body’s immune system. The team needed to design a micropatch large enough to trigger this response, but small enough to not impede their normal functions. These new micropatches they created, named Cyto-Adhesive Micro-Patches (CAMPs), are composed of two polymers and do not contain biologically active chemicals designed to be delivered into host cells. To aid the CAMPs’ attachment to neutrophils, they added a fragment of an antibody that would bind to a specific protein found on the cells’ surface.
When the CAMPs were mixed with fresh mouse neutrophils, they readily stuck to the cells without harming them. Both in the lab and when injected into mice, CAMP-bearing neutrophils rapidly released several molecules indicative of activation against immune threats. The team also discovered that CAMPs caused more than 4,000 genes in the neutrophils to be expressed differently than untreated neutrophils. Specifically, neutrophils with CAMPs expressed more genes associated with the anti-tumour state, and genes coding for pro-inflammatory cytokines.
When co-cultured, the CAMP-bearing neutrophils activated macrophages, NK cells, dendritic cells and CD8+ T cells. Similar experiments performed with human neutrophils in vitro saw similar effects, indicating these findings could translate to humans.
In vivo tumour tests
When CAMP-bearing neutrophils were injected into mice with melanoma, the levels of multiple inflammatory cytokines in the animal’s blood increased. Imaging tests revealed that the neutrophils migrated to the tumour site within four hours, which was also replicated in a breast cancer model. Neutrophils were also seen in high numbers in the animal’s spleen and tumour-draining lymph nodes. CD8+ T cells and NK cells in the blood, spleen and tumours were activated. Notably, in mice treated with non-CAMP neutrophils, these results were not observed.
Furthermore, the mice with melanoma that received CAMP-bearing neutrophils displayed a much slower tumour growth rate. Mice with breast cancer that received the treatment had a longer survival time, with complete regression of cancer achieved in 15 percent of the animals.
Combining treatments
The researchers combined this neutrophil treatment with standard checkpoint inhibitor drug ACTLA-4 and saw mice with melanoma display greatly reduced tumour growth and improved survival rates: 67 percent of the animals survived beyond 40 days and 33 percent achieved complete remission within 60 days.
These mice were rechallenged with another melanoma tumour and none developed cancer for a second time, showing that their immune systems had generated a robust anti-tumour memory response. Senior author Dr Samir Mitragotri, professor of bioengineering and Hansjörg Wyss Professor of Biologically Inspired Engineering at SEAS, explained: “Part of the beauty of this neutrophil-based cancer treatment is that it does not require any genetic engineering or modification of the therapeutic cells before they are infused, which can greatly cut down on the processing time for getting lifesaving treatments into patients bodies…It could even be administered at a patient’s bedside within hours, compared to the 14-16 days required for current cell therapy manufacturing techniques.”
The researchers noted that they incubated neutrophils with CAMPs for two hours before infusing them into mice, so further studies are required to determine how long treated cells can be maintained before infusion. Researchers at the Mitragotri lab are continuing to explore neutrophil’s ability to treat other cancers, including glioblastoma, and are using the micropatches to join different immune cell types together to improve their delivery to their target tissues.
Dr Don Ingber, Wyss Founding Core Faculty member, Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital, and Hansjörg Wyss Professor of Bioinspired Engineering at SEAS, said of the technology: “Its ability to produce potent anti-cancer effects without the need for expensive biotherapeutics or genetic engineering, using material properties alone, is both astounding from a scientific perspective and hugely important in terms of its potential clinical and commercial value.”
This study was published in Nature Biomedical Engineering.
References
1 Ng LG, Ostuni R, Hidalgo A. Heterogeneity of neutrophils. Nature Reviews Immunology. 2019 February 28 [2024 March 20]; 19(4):255-65. Available from: https://doi.org/10.1038/s41577‐019‐0141‐8
2 Laskay T, Moller S, Ohms M. An Attempt to Polarize Human Neutrophils Toward N1 and N2 Phenotypes in vitro. Frontiers in Immunology. 2020 April 28 [2024 March 20]; 11: 532. Available from: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00532/full
Related topics
Cancer research, Immuno-oncology, Immunotherapy
Related conditions
Cancer, Cancer Research