Identifying vascular disease associations
Posted: 11 April 2024 | Dr Mete Civelek (University of Virginia), Ellen Capon (Drug Target Review) | No comments yet
In this Q&A, Associate Professor Dr Mete Civelek shares insights from the University of Virginia’s exciting recent study identifying several potential therapeutic targets for accelerating translational research in cardiovascular disease treatment, with a focus on proteins associated with the extracellular matrix (ECM) secretion by smooth muscle cells (SMCs).
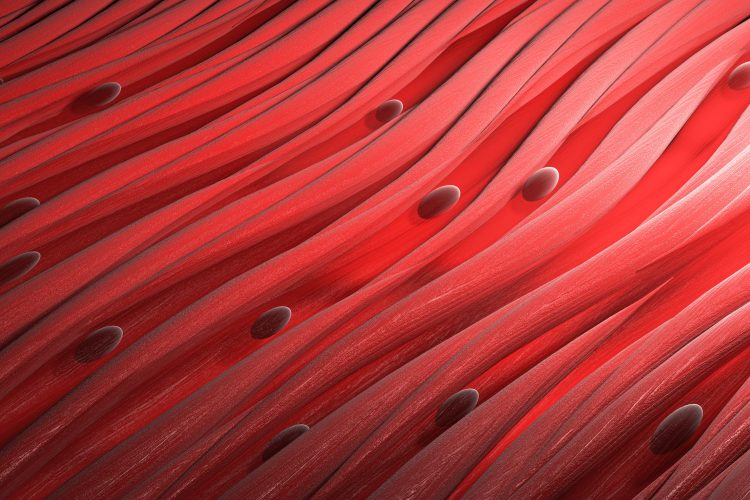
How do alterations in the microenvironment affect the phenotypic transition of smooth muscle cells (SMCs) from contractile to synthetic, and what implications does this have for cardiovascular health?
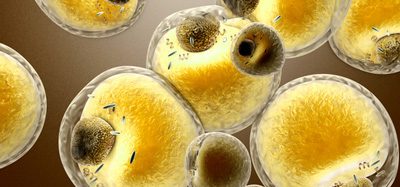
Alterations in the microenvironment can significantly influence the phenotypic transition of smooth muscle cells (SMCs) from a contractile to a synthetic state. The microenvironment encompasses various factors such as mechanical stress, biochemical signals, extracellular matrix (ECM) composition, and inflammatory mediators, among others. We specifically focused on the ECM in our publication because collagen, elastin, and fibronectin provide structural support and serve as signaling molecules. They also play an essential role in the stability of atherosclerotic plaques. Alterations in ECM composition can activate signaling pathways that promote the synthetic phenotype. Targeting pathways involved in SMC phenotypic modulation holds promise for developing novel therapeutic approaches for cardiovascular diseases. Strategies to modulate SMC phenotype towards a more contractile state may help prevent or reverse pathological vascular remodeling and improve cardiovascular outcomes.
Can you explain the methodology used to investigate the genetic variants regulating extracellular matrix (ECM) secretion in SMCs, and predict proteins associated with vascular disease?
We conducted a comprehensive investigation into the genetic regulation of extracellular matrix (ECM) secretion by smooth muscle cells (SMCs) and its implications for vascular diseases. We isolated human aortic SMCs from 123 multi-ancestry healthy heart transplant donors and cultured them to measure the abundance of secreted proteins using liquid chromatography–tandem mass spectrometry. We quantified 270 ECM and related proteins. We then performed protein quantitative trait locus (pQTL) mapping to identify genetic loci associated with variations in protein abundance. We then performed functional annotation of these loci through a colocalization approach, which helped prioritize genetic variants potentially linked to vascular disease risk. For example, this approach highlighted that the A allele of the rs6739323 variant at the 2p22.3 locus, associated with lower LTBP1 expression in SMCs and increased atherosclerosis and calcification risk. This multi-faceted methodology integrates proteomic analyses with genetic mapping to identify key proteins and genetic variants that could serve as novel therapeutic targets for vascular diseases.
Could you elaborate on the specific protein LTBP1 and its potential implications in improving plaque stability?
We identified LTBP1 (latent-transforming growth factor beta-binding protein 1) as a crucial protein in our study for its potential role in atherosclerotic plaque stability. The A allele of the genetic variant rs6739323 at the 2p22.3 locus is associated with reduced LTBP1 expression in smooth muscle cells (SMCs) and atherosclerosis-prone areas, correlating with an increased risk for SMC calcification. LTBP1 is abundant in SMCs, and its decreased expression is linked to advanced and unstable atherosclerotic plaque lesions, suggesting its pivotal role in maintaining plaque integrity. Previous studies support LTBP1’s involvement in ECM organization and TGF-beta activation, crucial for fibrous cap formation and stability. Thus, understanding LTBP1’s regulation and function could offer insights into strategies for enhancing plaque stability, potentially preventing plaque rupture and reducing the risk of cardiovascular events.
What potential therapeutic targets were identified for accelerating translational research in cardiovascular disease treatment?
Our study identified several potential therapeutic targets for accelerating translational research in cardiovascular disease treatment, with a focus on proteins associated with the extracellular matrix (ECM) secretion by smooth muscle cells (SMCs). Among these, LTBP1 (latent-transforming growth factor beta-binding protein) was highlighted due to its association with lower expression in SMCs and atherosclerosis-prone areas, correlated with increased SMC calcification risk. We identified additional 20 genetic loci associated with secreted protein abundance in SMCs, offering a broader range of potential targets. These findings pave the way for developing novel therapeutic strategies aimed at enhancing plaque stability and preventing cardiovascular events, by targeting the genetic and protein-level variations influencing ECM composition and function within vascular tissues.
What challenges might researchers face in translating these findings into clinical applications?
Translating our findings into clinical applications may face several challenges, including the complexity of genetic regulation of protein secretion and its implications for vascular disease. The specificity of the genetic variant rs6739323-A’s impact on LTBP1 expression and plaque stability needs thorough validation in additional model systems. The multifactorial nature of cardiovascular diseases complicates the direct application of single-target interventions. Moreover, developing therapies that modulate ECM composition without disrupting essential physiological processes presents a significant challenge. These factors underscore the necessity for extensive preclinical and clinical research to ensure safety and efficacy.
This study is published in Arteriosclerosis, Thrombosis, and Vascular Biology.
About the author


Dr Mete Civelek, Associate Professor, University of Virginia Department of Biomedical Engineering, a joint programme of UVA’s School of Medicine and School of Engineering.
Mete Civelek is an Associate Professor of Biomedical Engineering at the University of Virginia and is also a resident faculty at the UVA School of Medicine’s Center for Public Health Genomics. He is a member of the Robert M. Berne Cardiovascular Research Center and has a secondary appointment in the Department of Biochemistry and Molecular Genetics.
Related topics
Drug Targets, Genetic Analysis, Protein, Therapeutics
Related conditions
Cardiovascular disease