SPNS1 mutations reveal new lysosomal lipid recycling pathway
Posted: 17 October 2025 | Drug Target Review | No comments yet
Scientists have linked rare mutations in SPNS1 to a previously unknown lipid recycling pathway in lysosomes, revealing how faulty fat processing can trigger muscle and liver disease.
Researchers have traced a rare multi-organ disorder to mutations in the gene SPNS1, which block lysosomal lipid recycling. The discovery identifies a new pathway in fat metabolism with implications for lysosomal storage diseases and potential therapeutic development.
As Deputy Director of the Cardiovascular & Metabolic Disorders Programme at Duke-NUS Medical School, Professor David Silver describes how his team identified SPNS1’s role in lysosomal lipid recycling, the consequences of pathway failure and the wider implications for future therapies.
A career at the crossroads of biochemistry and disease
Professor Silver’s research has long centred on lipids – the essential molecules that form cell membranes and regulate energy. He describes his focus simply: “I’m a Biochemist and Professor at Duke-NUS Medical School. My lab primarily focuses on the study of transport proteins and enzymes often important in diseases such metabolic, cardiovascular and neurological diseases.”
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
An earlier milestone for Silver, before identifying SPNS1’s role in lipid recycling, was the discovery of MFSD2A – a lipid transporter that carries omega-3 fatty acids into the brain. This finding provided key insights into how nutrient transport influences human development and formed the basis for the group’s later focus on SPNS1.
Identification of MFSD2A
Commenting on his foundational work, Silver says: “Our team previously discovered the lipid transporter MFSD2A, which is a lysophospholipid (LPL) transporter that brings omega-3 fatty acids, among other fatty acids linked to the LPC molecule, into the brain. Among our earlier studies with our clinical collaborators, we characterised inactivating variants in MFSD2A in patients with severe microcephaly, indicating that MFSD2A is essential for human brain development.”
Among our earlier studies with our clinical collaborators, we characterised inactivating variants in MFSD2A in patients with severe microcephaly, indicating that MFSD2A is essential for human brain development.
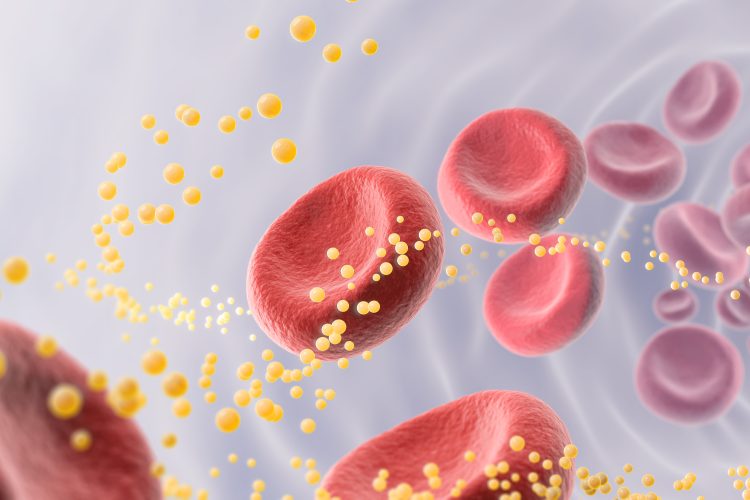
LPC, or lysophosphatidylcholine, is produced when phosphatidylcholine – the most abundant phospholipid in cell membranes – is broken down. It also acts as a carrier for fatty acids in the bloodstream.
Drawing on historical work by Nobel laureate Christian de Duve, Silver’s group hypothesised that lysosomes – the cell’s ‘recycling centres’ – might contain a parallel transporter for lysophospholipids. Their search led them to SPNS1.
“Using biochemical assays, cell-based models including patient-derived fibroblasts, we were able to definitively demonstrate that the SPNS1 variants in our study patients led to a build-up of lysosomal lipids including LPC and cholesterol.”
The findings dovetailed with previous in vivo research linking SPNS1 deficiency to tissue damage in liver and muscle.
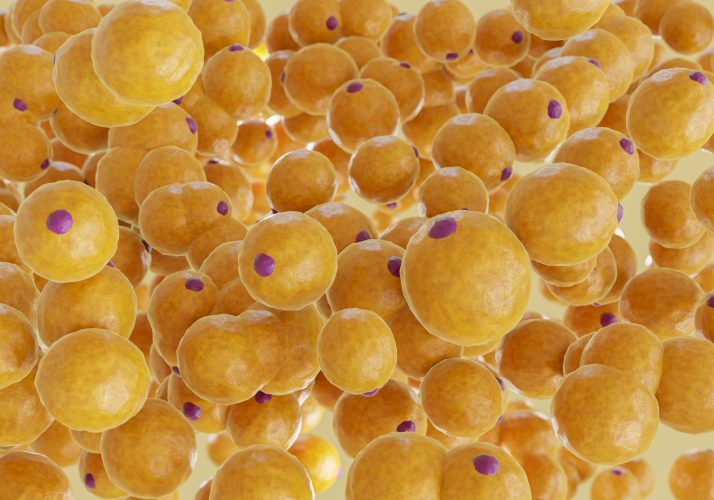
Lipid accumulation, as seen in fat cells, mirrors the cellular buildup caused by loss of SPNS1 function, revealing a new pathway in fat metabolism and disease. Image credit: Shutterstock / Daecheol
Faulty fat recycling and cellular stress
SPNS1’s role is to remove LPC from lysosomes. When mutations block this process, the consequences are far-reaching.
SPNS1 is essential for the removal of LPC from lysosomes. The patients in our study have inactivating variants in SPNS1 leading to the build-up of LPC and cholesterol within their lysosomes.
“SPNS1 is essential for the removal of LPC from lysosomes. The patients in our study have inactivating variants in SPNS1 leading to the build-up of LPC and cholesterol within their lysosomes.”
This lipid overload disrupts how cells respond to stress, particularly under nutrient deprivation.
“Some of our biochemical findings suggest that cells without normal SPNS1 function could be maladaptive to nutrient deprivation because of the inability to export LPC from lysosomes, which we found directly contributed to the storage of excess triglyceride within cells in conditions that mimicked nutrient deprivation.”
Lysosomal storage diseases
The discovery of SPNS1-mediated lipid recycling broadens the picture of lysosomal storage diseases – a group of disorders marked by defective breakdown and clearance of cellular waste.
Our study of SPNS1 function reveals a new pathway by which the cell recycles the most abundant class of phospholipids.
“Our study of SPNS1 function reveals a new pathway by which the cell recycles the most abundant class of phospholipids. These are early days in the study of this newly revealed pathway and more work needs to be done to fully understand how SPNS1 deficiency leads to the disease we reported in our study.”
By demonstrating how LPC recycling intersects with cholesterol handling, Silver’s team has identified new directions for mechanistic research and therapeutic exploration.
The challenges of rare disease drug discovery
For ultra-rare disorders like SPNS1 deficiency, translating discoveries into therapies presents significant challenges.
“Some of the key challenges that need to be overcome before development of therapies is to have a clear gene–disease association established, including functionalisation of variants and underlying mechanisms causing disease,” Silver explains.
Even when the science is sound, access to technology is not guaranteed.
“These challenges can usually be met but the science often comes up against other equally important challenges such as access to affordable therapeutic technologies for rare disease – some of which are not new but are expensive to access and could involve regulatory hurdles that are difficult to navigate.”
Wider implications for lipid metabolism
While only a small number of patients are known to be affected by SPNS1 variants, the findings provide insights into core biological processes that may inform understanding of more common diseases.
One of the surprising findings from our study was that LPC transport is important for cholesterol transport from lysosomes. More research will be needed to understand this connection.
“I think there are several lessons we learned from our study that expand our understanding of the physiological roles SPNS1-mediated phospholipid salvage plays in the cell. For example, one of the surprising findings from our study was that LPC transport is important for cholesterol transport from lysosomes. More research will be needed to understand this connection,” Silver reflects.
Understanding these interlinked pathways could ultimately enrich knowledge of metabolic regulation, lipid-associated disorders and cardiovascular risk.
Next steps for SPNS1 research
For Silver and colleagues, the path forwards involves both deepening mechanistic insight and exploring therapeutic feasibility.
“Our study provides a compelling case based on our biochemical findings that the SPNS1 patients in our study would benefit from gene therapy,” he says. “At the same time, an important next step in SPNS1 research will be to better understand how SPNS1 inactivation leads to liver and muscle disease.”
With rare disease research increasingly intersecting with emerging technologies such as gene therapy and RNA-based interventions, SPNS1 could serve as a valuable test case for how academic discovery connects with clinical translation.
Conclusion: small genes, big lessons
Professor Silver’s research illustrates how studies of rare, ultra-specific mutations can provide insights with wide biological and therapeutic significance. SPNS1 deficiency is extremely uncommon, yet defining its role in lipid recycling advances understanding of lysosomal biology and metabolic regulation.
As the drug discovery community continues to address the scientific and economic challenges of rare disease research, Silver’s findings provide a framework for rigorous mechanistic investigation. The next phase will require deeper study of SPNS1 in health and disease alongside collaborative efforts to overcome translational barriers in ultra-rare conditions.
Meet the expert


His long-standing research interests are in lipid storage, transport and metabolism, with a translational focus on applying his laboratory’s discoveries to the treatment of human diseases.
Dr Silver’s notable discoveries include the FITM family of endoplasmic reticulum proteins, Mfsd2a – a lysolipid transporter critical for human brain growth – and SPNS1, a lysosomal lysolipid transporter important for phospholipid salvage and lysosomal function.
Image of Dr Silver courtesy of Duke-NUS Medical School.
Related topics
Analysis, Assays, Drug Discovery Processes, Gene Therapy, Genetic Analysis, Lipidomics, Lipids, Metabolomics, Sequencing
Related conditions
Lysosomal storage diseases, SPNS1 deficiency
Related organisations
Duke-NUS Medical School