Why do we have no effective treatments for osteoarthritis?
Posted: 20 April 2019 | Pradeep Sacitharan | No comments yet
Osteoarthritis (OA) is a painful and debilitating disease of articular joints.1,2 Its clinical prevalence is as high as 21.6 percent of the population in the United States,3 which constitutes direct health costs of over 80 billion US dollars annually.4
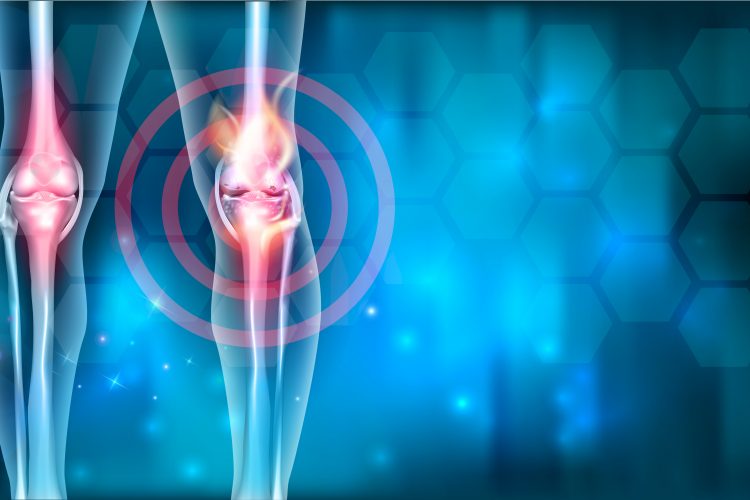
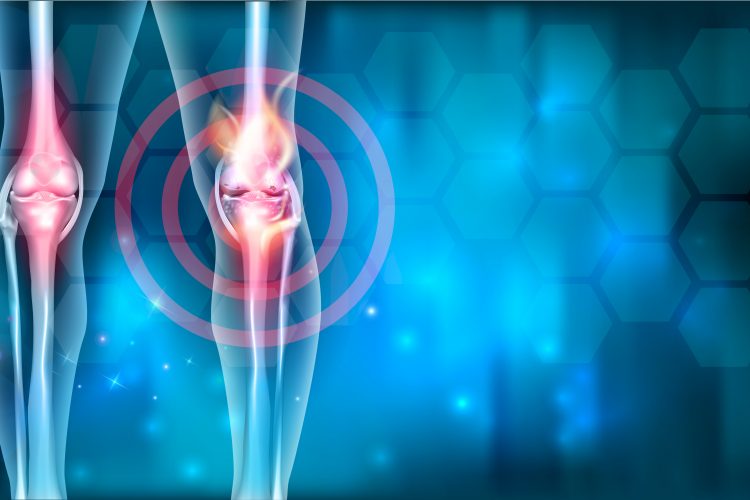
Due to the increasing mean age of the global population, it is believed that OA will become the fourth leading cause of disability worldwide by 2020.5 Symptoms vary from moderate pain to disability – which in turn can lead to low mood and depression6 – as well as progressive cartilage loss, subchondral bone thickening, osteophyte formation and joint space narrowing.2 Growing evidence implicates the impairment of several physiological mechanisms in the pathogenesis of OA,7-9 and despite these recent advances in understanding the pathogenesis of OA thus far, they have failed to deliver any disease-modifying therapeutics.
Current therapeutics
Depending on the severity of OA, patients are firstly advised to lose weight and modify their lifestyles through diet and exercise.10 Use of supplements including glucosamine and chondroitin is common; however, the efficacy of these supplements remains controversial.11 Topical creams are also used to reduce local pain, but patients are usually initially prescribed oral paracetamol and/or non-steroidal anti-inflammatory drugs.12 Further treatment involves intra-articular injections of corticosteroids, hyaluronic acid or biologics (and new intra-articular injectable drugs are in the pipeline).13 The end-point treatment for OA remains that of joint replacement surgery,14 which offers less pain and improvements in physical function, yet many patients don’t reach the comparable mobility level of their population peers.14 Furthermore, a person’s age and state of health (ie, any comorbidities) may exclude them from joint replacement surgery, particularly when further surgery is required on other joints or the same joint in the future.15 Hence, more research is required to find effective therapies to tackle OA.
Challenges in drug discovery
Unlike the case of rheumatoid arthritis, where TNF-α inhibitors have been blockbuster successes, there are no precise causative targets in OA (that we know of) that will have the same impactful therapeutic benefit.16 The lack of effective targets makes OA drug discovery highly challenging and less attractive. In addition, the OA field has reached a consensus that the disease has different patient subsets that require greater classification and will impact drug discovery in the future.17 Another challenge is translating pre-clinical modelling data into human clinical trials. The field has made progress in the last two decades in establishing disease models of cartilage degradation, ageing, pain and joint injuries; but these models are not readily translating the benefits seen in vivo to man.18 The final challenge remains that of endpoints in clinical trials. Disease biomarkers are lacking, and patient-reported outcomes are not reliable (high placebo effects),19 producing data with a high degree of variability.20 Furthermore, the slow progressive and unpredictable nature of the disease means trials are not cost effective.
What we must achieve together
Conclusions
In all, we need to chip away together on four main goals: (i) better patient stratification for disease phenotyping; (ii) development of imaging-based efficacy endpoints; (iii) diversifying the use of animal models in basic science; and (iv) finding better biomarkers for different patient subsets. I am in awe of the myriad drug discoveries that have been made and ask myself ‘why not in OA?’. I am optimistic that major breakthroughs in the quest for effective OA treatments will come in my lifetime.
Biography


References
- Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. Lancet [Internet]. 2011 Jun 18 [cited 2014 Mar 21];377(9783):2115–26. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21684382
- Glyn-Jones S, Palmer AJR, Agricola R, Price AJ, Vincent TL, Weinans H, et al. Osteoarthritis. Lancet [Internet]. 2015;386(9991):376–87. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0140673614608023
- Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the united states: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Archives of Physical Medicine and Rehabilitation. 2014.
- Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–56.
- Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;
- Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol [Internet]. 2011;7(1):33–42. Available from: http://dx.doi.org/10.1038/nrrheum.2010.196
- Sacitharan PK, Vincent TL. Cellular ageing mechanisms in osteoarthritis. Mamm Genome [Internet]. 2016;27(7):421–9. Available from: http://dx.doi.org/10.1007/s00335-016-9641-z
- Mobasheri A, Rayman MP, Gualillo O, Sellam J, Van Der Kraan P, Fearon U. The role of metabolism in the pathogenesis of osteoarthritis. Nature Reviews Rheumatology. 2017.
- Yusuf E. Pharmacologic and Non-Pharmacologic Treatment of Osteoarthritis. Curr Treat Options Rheumatol. 2016
- Wieland HA, Michaelis M, Kirschbaum BJ, Rudolphi KA. Osteoarthritis – an untreatable disease? Nat Rev Drug Discov [Internet]. 2005 Apr [cited 2014 Mar 19];4(4):331–44. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15803196
- Cheng DS, Visco CJ. Pharmaceutical therapy for osteoarthritis. PM R [Internet]. 2012 May [cited 2014 Apr 22];4(5 Suppl):S82-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22632707
- Thysen S, Luyten FP, Lories RJU. Targets, models and challenges in osteoarthritis research. Dis Model Mech. 2015
- OARSI. Osteoarthritis: A Serious Disease, Submitted to the U.S. Food and Drug Administration. Oarsi [Internet]. 2016; Available from: https://www.oarsi.org/sites/default/files/docs/2016/oarsi_white_paper_oa_serious_disease_121416_1.pdf
- Fang M, Noiseux N, Linson E, Cram P. The Effect of Advancing Age on Total Joint Replacement Outcomes. Geriatr Orthop Surg Rehabil. 2015.
- Calich ALG, Domiciano DS, Fuller R. Osteoarthritis: Can anti-cytokine therapy play a role in treatment? Clin Rheumatol. 2010;29(5):451–5.
- Kraus VB, Blanco FJ, Englund M, Karsdal MA, Lohmander LS. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthritis and Cartilage. 2015.
- Fang H, Beier F. Mouse models of osteoarthritis: modelling risk factors and assessing outcomes. Nat Rev Rheumatol [Internet]. 2014 Jul [cited 2014 Jul 15];10(7):413–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24662645
- Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, McAlindon TE. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: A systematic review and network meta-analysis. Annals of Internal Medicine. 2015.
- McAlindon TE, Driban JB, Henrotin Y, Hunter DJ, Jiang GL, Skou ST, et al. OARSI Clinical Trials Recommendations: Design, conduct, and reporting of clinical trials for knee osteoarthritis. Osteoarthritis and Cartilage. 2015.
- Berenbaum F. Deep phenotyping of osteoarthritis: a step forward. Ann Rheum Dis [Internet]. 2019 Jan 1;78(1):3 LP-5. Available from: http://ard.bmj.com/content/78/1/3.abstract
- Little CB, Hunter DJ. Post-traumatic osteoarthritis: from mouse models to clinical trials. Nat Rev Rheumatol. 2013;9(8):485–97.
- Cope PJ, Ourradi K, Li Y, Sharif M. Models of osteoarthritis: the good, the bad and the promising. Osteoarthr Cartil [Internet]. 2019 Feb 1 [cited 2019 Jan 29];27(2):230–9. Available from: https://www.sciencedirect.com/science/article/pii/S1063458418315073
- Lotz M, Martel-Pelletier J, Christiansen C, Brandi ML, Bruyère O, Chapurlat R, et al. Value of biomarkers in osteoarthritis: current status and perspectives. Ann Rheum Dis [Internet]. 2013 Nov 1 [cited 2019 Jan 29];72(11):1756–63. Available from: https://ard.bmj.com/content/72/11/1756
Related topics
Assays, Drug Discovery, Screening, Therapeutics
Related conditions
Osteoarthritis
Related organisations
Liverpool University