Novel nanoparticles deliver innovative cancer chemoimmunotherapy
Posted: 1 December 2022 | Izzy Wood (Drug Target Review) | No comments yet
University of Pittsburgh researchers have designed cancer-fighting nanoparticles that co-deliver a chemotherapy drug and a novel immunotherapy
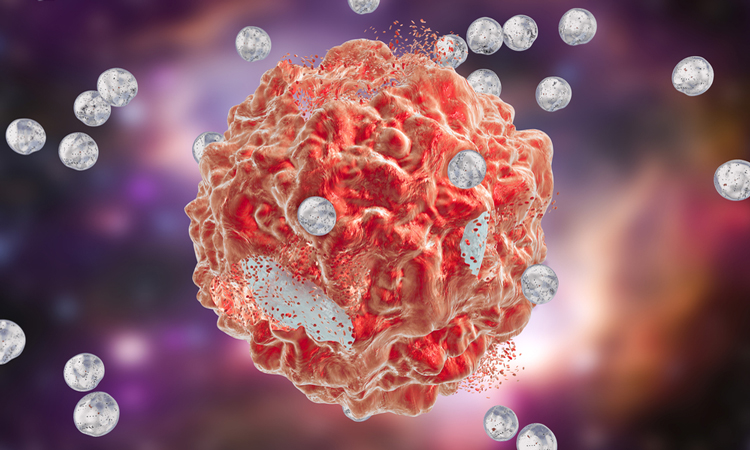
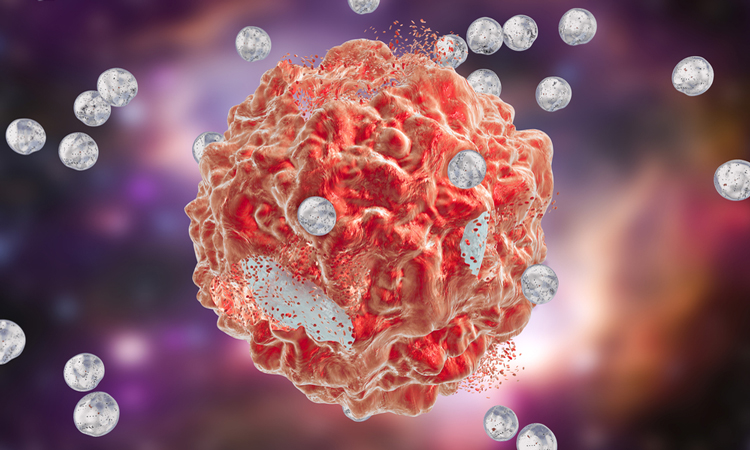
University of Pittsburgh researchers, US, have designed a new immunotherapy approach that silences a gene involved in immunosuppression. When combined with an existing chemotherapy drug and packaged into tiny nanoparticles, the therapy shrunk tumours in mouse models of colon and pancreatic cancer.
This immunotherapy process, published in Nature Nanotechnology, involved a lipid called phosphatidylserine (PS), which is usually found inside the tumour cell membrane’s inner layer but migrates to the cell surface in response to chemotherapy drugs. On the surface, PS acts as an immunosuppressant, protecting remaining cancer cells from the immune system.
The Pitt researchers found that treatment with chemotherapy drugs fluorouracil and oxoplatin (FuOXP) led to increased levels of Xkr8, a protein that controls distribution of PS on the cell membrane. This finding suggested that blocking Xkr8 would prevent cancer cells from shunting PS to the cell surface, allowing immune cells to eliminate cancer cells that lingered after chemotherapy.
The team designed snippets of genetic code called short interference RNA (siRNA), which shuts down production of Xkr8. After packaging siRNA and FuOXP together into dual-action nanoparticles, the next step was targeting them to tumours.
Nanoparticles are typically too large to cross intact blood vessels in healthy tissue, but they can reach cancer cells because tumours sometimes have poorly developed vessels with holes that allow them passage. But this tumour-targeting approach is limited because many human tumours do not have large enough holes for nanoparticles to pass through.
CHECK THIS OUT: Nanotechnology platform sensitises cancer to immunotherapy
A new pre-clinical study has utilised nanoparticles to attach immune-activating molecules to cancer cells.