Likely link found between Zika virus and microcephaly
Posted: 4 March 2016 | Victoria White | No comments yet
Working with lab-grown human stem cells, a team of researchers suspect they have discovered how the Zika virus probably causes microcephaly in foetuses…
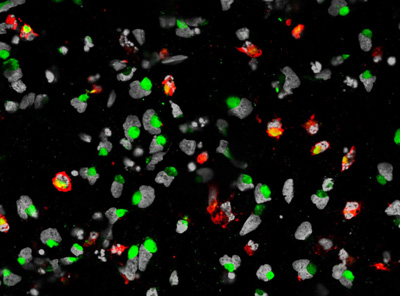
This image shows cell death of the human neural progenitor cells (hNPCs) is mark by cleaved caspase 3 in red, the nuclei of hNPCs are labeled by DAPI in white/grey, and the ZIKA virus is labeled by ZIKA virus envelope protein in green. CREDIT: Sarah C. Ogden
Working with lab-grown human stem cells, a team of researchers suspect they have discovered how the Zika virus probably causes microcephaly in foetuses.
They believe that the virus selectively infects cells that form the brain’s cortex, making them more likely to die and less likely to divide normally and make new brain cells.
The researchers say their experiments also suggest these highly-susceptible lab-grown cells could be used to screen for drugs that protect the cells or ease existing infections.
“Studies of foetuses and babies with the tell-tale small brains and heads of microcephaly in Zika-affected areas have found abnormalities in the cortex, and Zika virus has been found in the foetal tissue,” says Guo-li Ming, M.D., Ph.D., a professor of neurology, neuroscience, and psychiatry and behavioural science at Johns Hopkins‘ Institute for Cell Engineering. “While this study doesn’t definitely prove that Zika virus causes microcephaly, it’s very telling that the cells that form the cortex are potentially susceptible to the virus, and their growth could be disrupted by the virus.”
Ming led the research team along with Hongjun Song, Ph.D., a professor of neurology and neuroscience in the Institute for Cell Engineering, and Hengli Tang, Ph.D., a virologist at Florida State University.
In a quickly executed study that reflects the global public health threat posed by Zika, the researchers compared Zika’s effect on cells known as cortical neural progenitor cells to two other cell types: induced pluripotent stem cells and immature neurons. Induced pluripotent stem cells are made by reprogramming mature cells, and can give rise to any cell type in the body, including cortical neural progenitor cells. Cortical neural progenitor cells in turn give rise to immature neurons.
The experiments, conducted in less than a month, began when Tang reached out to Ming and Song, who use stem cells to study early brain development. The Johns Hopkins labs sent team members and cells to Tang’s lab, where the cells were exposed to Zika virus. Then the cells’ genetic expression were analysed in Peng Jin’s laboratory at Emory University.
90% of the cortical neural progenitor cells were infected after three days
According to Tang, three days after exposure to the virus, 90% of the cortical neural progenitor cells were infected, and had been hijacked to churn out new copies of the virus. Furthermore, the genes needed to fight viruses had still not been switched on, which is highly unusual, he adds. Many of the infected cells died, and others showed disrupted expression of genes that control cell division, indicating that new cells could not be made effectively.
Using specific, known types of cells allowed the researchers to see where the developing brain is most vulnerable, Song says. He and Ming are now using the cells to find out more about the effects of Zika infection on the developing cortex.
“Now that we know cortical neural progenitor cells are the vulnerable cells, they can likely also be used to quickly screen potential new therapies for effectiveness,” Song adds.