A promising new treatment strategy for hepatoblastoma
Posted: 22 February 2024 | Drug Target Review | No comments yet
A combination therapy of vincristine, irinotecan and panobinostat, tested in high-risk, relapsed or refractory HB spheroids, decreased tumour marker levels.
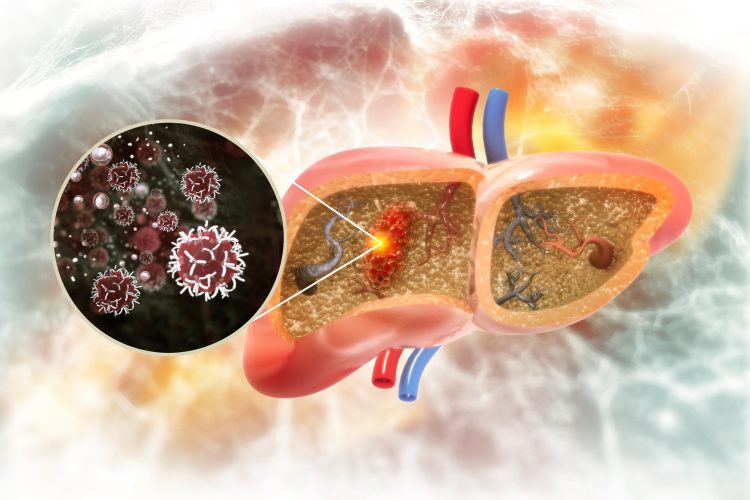
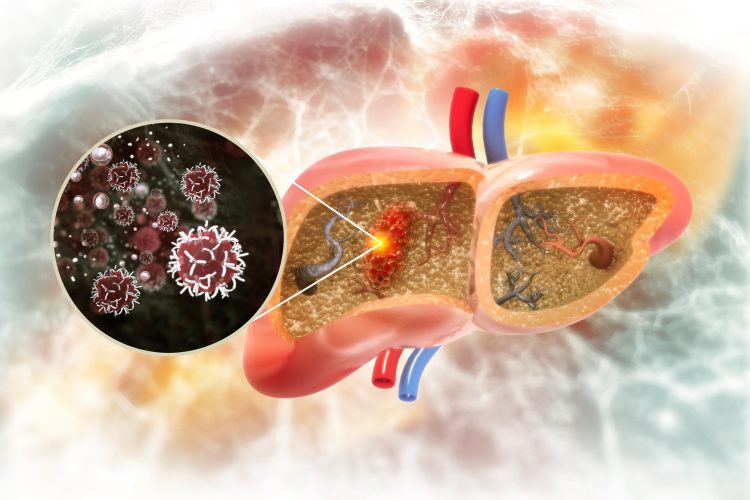
Led by Baylor College of Medicine, a team of researchers have reported a novel treatment strategy for hepatoblastoma (HB), the most common liver cancer in children. In the last decade, HB has been rising rapidly worldwide and has seen the most rapid increase among all paediatric solid tumours.
Dr Andrés Espinoza, general surgery resident in Baylor’s Michael E. DeBakey Department of Surgery, commented: “High-risk disease leads to high rates of relapse and mortality.” This highlights the need for an effective therapeutic approach.
Dr Espinoza continued: “In this study, we investigated the potential benefits of a new combination therapy that included an inhibitor of the enzyme histone deacetylase (HDAC) present at elevated levels in HB cells…Previous studies have suggested that HDAC inhibitors may provide treatment options for HB, but there is no published preclinical data on such therapies.”
The scientists developed a preclinical testing pipeline with clinically relevant HB models. First, they tested several HDAC inhibitors on their ability to kill patient-derived HB cell lines grown in the lab and discovered that HDAC inhibitor panobinostat was the most effective at eliminating cancer cells.
Following that, the team assessed whether adding panobinostat to current chemotherapy regimens would improve tumour response. They screened these treatments in patient-derived spheroids, and the findings demonstrated that adding panobinostat to the combination treatment including vincristine and irinotecan eliminated more tumour cells than any of the other combinations.
The final test was to assess the new combination therapy of vincristine, irinotecan and panobinostat (VIP) in four aggressive animal models of HB the researchers had derived from high-risk, relapsed and treatment refractory HBs. The molecular characterisation of these tumours in the animal models showed that they conserved all mutations found in the human tumours of origin, as well as other molecular markers present in patient tumour samples. This indicated that the tumours in the animal models closely matched those in the patients. Notably, this study tested VIP in large tumours, whereas other studies have tested treatments on small-sized tumours.
Corresponding author and associate professor of surgery at Baylor Dr Sanjeev Vasudevan explained: “After just one week of therapy, the tumours that were treated with VIP had a significant decrease in volume and alpha fetoprotein levels, the tumour marker.” He concluded: “These findings are very encouraging as they suggest that VIP therapy may be a promising and effective option for patients with currently untreatable high-risk, relapsed or refractory HB.”
This study was published in the Journal of Hepatology.
Related topics
Cancer research, Cell Line Development, Oncology, Spheroids
Related conditions
Cancer Research, Hepatoblastoma
Related organisations
Baylor College of Medicine