Nano-medicine inhibits progression of pancreatic cancer
Posted: 3 January 2018 | Dr Zara Kassam (Drug Target Review) | No comments yet
Survival rates in pancreatic cancer linked to the inverse correlation between specific oncogene and tumour suppressant microRNA…
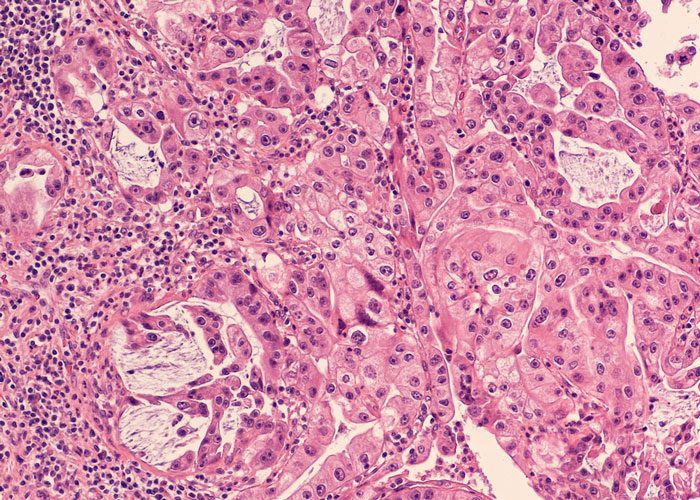
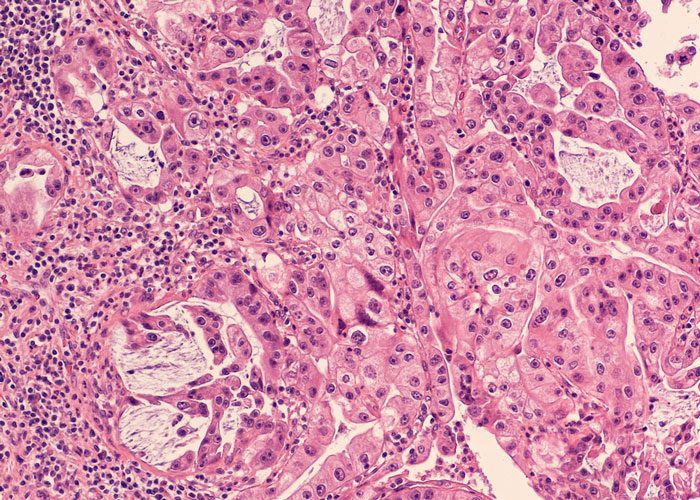
Researchers have examined pancreatic cancer cells and discovered an inverse correlation between the signatures of miR-34a, a tumour suppressant, and PLK1, a known oncogene.
The levels of miR-34a were low in pancreatic cancer mouse models, while the levels of the oncogene were high. This correlation made sense for such aggressive cancer. The research team now needed to see if the same was true in humans.
The scientists performed RNA profiling and analysis of samples taken from pancreatic cancer patients. The molecular profiling revealed the same genomic pattern found earlier in mouse models of pancreatic cancer.
The scientists then devised a novel nanoparticle that selectively delivers genetic material to a tumour and prevents side effects in surrounding healthy tissues.
“We designed a nano-carrier to deliver two passengers: (1) miR-34a, which degrades hundreds of oncogenes; and (2) a PLK1 small interfering RNA (siRNA), that silences a single gene,” said Professor Satchi-Fainaro, Chair of the Department of Physiology and Pharmacology at Tel Aviv University‘s Sackler Faculty of Medicine. “These were delivered directly to the tumour site to change the molecular signature of the cancer cells, rendering the tumour dormant or eradicating it altogether.
“The nanoparticle is like a taxi carrying two important passengers,” Prof. Satchi-Fainaro continues. “Many oncology protocols are cocktails, but the drugs usually do not reach a tumour at the same time. But our ‘taxi’ kept the ‘passengers’ — and the rest of the body — safe the whole way, targeting only the tumour tissue. Once it ‘parked,’ an enzyme present in pancreatic cancer caused the carrier to biodegrade, allowing the therapeutic cargo to be released at the correct address — the tumour cells.”
To validate their findings, the scientists injected the novel nanoparticles into pancreatic tumour-bearing mice and observed that by balancing these two targets — bringing them to a normal level by increasing their expression or blocking the gene responsible for their expression — they significantly prolonged the survival of the mice.
“This treatment takes into account the entire genomic pattern and shows that affecting a single gene is not enough for the treatment of pancreatic cancer or any cancer type in general,” according to Prof. Satchi-Fainaro.
Pancreatic cancer is among the most aggressive cancers known today. The overwhelming majority of pancreatic cancer patients die within just a year of diagnosis. “Despite all the treatments afforded by modern medicine, some 75% of all pancreatic cancer patients die within 12 months of diagnosis, including many who die within just a few months,” Prof. Satchi-Fainaro says.
“But around seven percent of those diagnosed will survive more than five years. We sought to examine what distinguishes the survivors from the rest of the patients,” Prof. Satchi-Fainaro continues. “We thought that if we could understand how some people live several years with this most aggressive disease, we might be able to develop a new therapeutic strategy.”
The study has been published in Nature Communications.
Related topics
Drug Development, miRNAs, Oncology
Related conditions
Pancreatic cancer
Related organisations
Tel Aviv University
Related people
Dr Shay Eliyahu, Hadas Gibori, Professor Ronit Satchi-Fainaro