First blood-brain barrier chip using stem cells developed
Posted: 13 June 2019 | Drug Target Review | No comments yet
Researchers have, for the first time, duplicated a patient’s blood-brain barrier (BBB), creating a human BBB chip with stem cells.
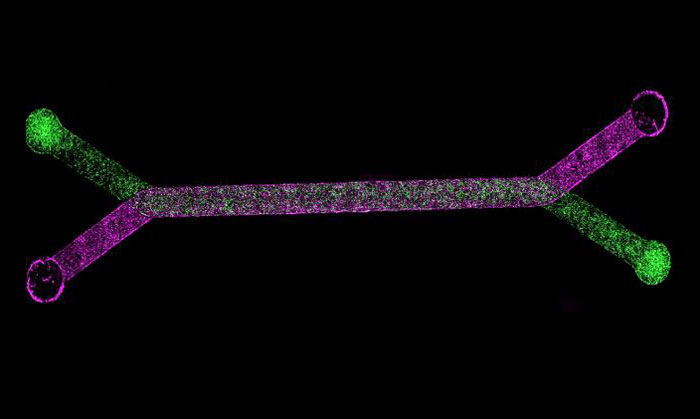
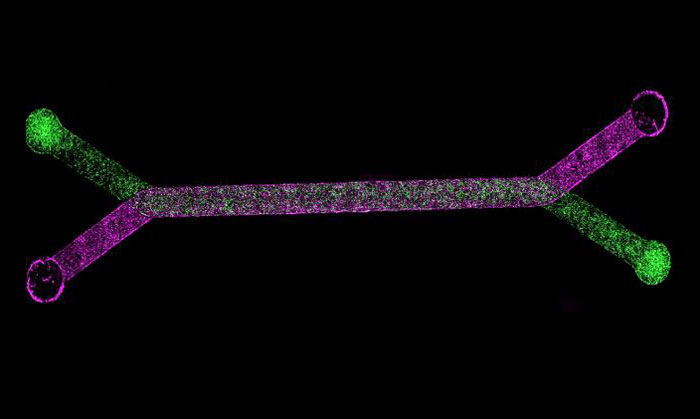
Genetically manipulated blood cells are placed on a microfluidic organ-chip developed by Emulate (above) approximately the size of an AA battery, which contains tiny hollow channels lined with tens of thousands of living human cells and tissues (credit: Dr Gad Vatine/BGU).
The research, which is a collaboration between Dr Gad Vatine of BGU’s Regenerative Medicine and Stem Cell Research Centre and Department of Physiology and Cell Biology and Dr Clive N Svendsen, of Cedars-Sinai Medical Center in Los Angeles, can be used to develop personalised medicine and new techniques to research brain disorders.
For the study, the researchers genetically manipulated blood cells into pluripotent stem cells. These were used to create the various cells that comprise the blood-brain barrier. The cells were then placed on a microfluidic BBB organ-chip, which contained tiny hollow channels lined with tens of thousands of living human cells and tissues, which re-creates the natural physiology and mechanical forces that cells experience within the human body. The living cells then re-created a functioning BBB, including blocking the entry of certain drugs.
Significantly, when this blood-brain barrier was derived from cells of patients with Allan-Herndon-Dudley syndrome, a rare congenital neurological disorder, and Huntington’s disease patients, the barrier malfunctioned in the same way that it does in patients with these diseases.
“By combining patient-specific stem cells and organ-on-chip technology, we generated a personalised model of the human BBB,” said Dr Vatine. “BBB-on-chips generated from several individuals allows the prediction of the best suited brain drug in a personalised manner. The study’s findings create dramatic new possibilities for precision medicine.”
This is of particular importance for neurological diseases like epilepsy or schizophrenia. “By combining organ-chip technology and human iPSC-derived tissue, we have created a neurovascular unit that recapitulates complex BBB functions, providing a platform for modeling inheritable neurological disorders, and advances drug screening, as well as personalised medicine,” Dr Vatine explained.
The research was published in the journal Cell Stem Cell.
Related topics
Cell Cultures, Personalised Medicine, Precision Medicine, Research & Development, Stem Cells
Related organisations
Ben-Gurion University of the Negev (BGU), Cedars-Sinai Medical Center
Related people
Dr Gad Vatine