Children produce a different antibody response to SARS-CoV-2 infection, finds study
Posted: 6 November 2020 | Hannah Balfour (Drug Target Review) | 1 comment
A new analysis reveals that the course of SARS-CoV-2 infection and the immune response it provokes is completely different in adults and children.
Researchers have found that children and adults produce different types and amounts of antibodies in response to SARS-CoV-2 infection, suggesting that the course of infection and immune response is completely different in these two age groups.
“Our study provides an in-depth examination of SARS-CoV-2 antibodies in kids, revealing a stark contrast with adults,” said Columbia University Vagelos College of Physicians and Surgeons immunologist Dr Donna Farber, the George H. Humphreys II Professor of Surgical Sciences in the Department of Surgery, who led the study with Dr Matteo Porotto, associate professor of viral molecular pathogenesis in Columbia’s Department of Pediatrics.
Children are less affected by SARS-CoV-2 infections
According to the team, one of the surprising manifestations of the COVID-19 pandemic is that most children combat the infection with very few issues, while older people struggle. Infection with the SARS-CoV-2, the virus that causes COVID-19, prompts adults to develop respiratory symptoms which can become severe and result in acute respiratory distress syndrome (ARDS). Children, on the other hand, are largely spared from respiratory illness, but can develop multisystem inflammatory syndrome (MIS-C) which is life-threatening.
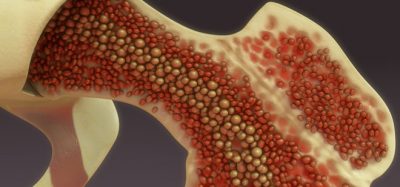
“This is a new infection for everybody, but children are uniquely adapted to see pathogens for the first time. That is what their immune system is designed to do. Children have a lot of naive T cells that are able to recognise all sorts of new pathogens, whereas older people depend more on their immunological memories. We are not as able to respond to a new pathogen…” Faber said.
Children produce fewer neutralising antibodies
In their paper, researchers studied 47 children – 16 treated for MIS-C and the other 31 with confirmed COVID-19 but no MIS-C – and 32 adults with symptoms ranging from milder disease (patients able to recover at home) to those hospitalised with severe COVID-19. According to the team, half of the children without MIS-C had no COVID-19 symptoms.
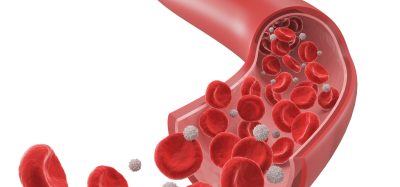
In their analysis, children with or without MIS-C produced the same antibody profile, but this profile was different from that found in the adults.
The children had fewer antibodies targeting the SARS-CoV-2 Spike (S) protein which the virus uses to infect human cells. The children’s antibodies also had the least neutralising activity, while all adults produced neutralising antibodies. The antibodies found in the sickest adults had the most neutralising activity.
Farber stated that the sickest individuals having the most neutralising antibodies likely reflects the amount of time the virus is present in the sickest patients: “There is a connection between the magnitude of your immune response and the magnitude of the infection: The more severe the infection, the more robust the immune response, because you need to have more immune cells and immune reactions to clear a higher dose of a pathogen.”
Farber also said that the fact that children produce very few antibodies targeting the S protein suggests that the infection does not spread a lot or damage a lot of their cells. Porotto added: “Because children clear the natural virus rapidly, they do not have a widespread infection and they do not need a strong antibody response.”
The team suggest that this reduced course of infection in children may indicate that they are infectious for a shorter period of time, compared with adults, and therefore less likely to spread the virus, although the researchers did not measure viral load in the children.
“Current studies in other countries indicate that younger school-age children are not vectors for the new coronavirus, so our data are consistent with those findings,” Farber said.
Children should still respond well to SARS-CoV-2 vaccines
The researchers said that despite producing fewer antibodies in response to SARS-CoV-2 infection, children should not have a weaker response to a future vaccine, as the vaccines under development do not mimic the normal route of infection.
“Even though children do not produce neutralising antibodies in response to a natural infection with SARS-CoV-2, vaccines are designed to generate a protective immune response in the absence of an infection,” Farber explained. “Children respond very well to vaccines, and I think they will develop good neutralising antibody responses to a SARS-CoV-2 vaccine, they will probably be better protected than the adults.
Future focus: what does the adult immune system lack?
While the study suggests that the course of infection is different for adults and children, why this is the case is still unclear. The researchers at Columbia now want to understand why children clear SARS-CoV-2 more easily and what may be lacking in the adult immune system, stopping them from doing the same.
Farber, Porotto and their colleagues are currently looking for differences in T-cell response, especially T cells that reside in the lung. Previous research from Farber’s lab has shown these T cells which inhabit tissue are more important in fighting lung infections than T cells that circulate via the bloodstream.
The team suggest that children may generate a stronger immune response to SARS-CoV-2 infections, deploying interferon and macrophages to indiscriminately attack cells infected by pathogens. While other studies have indicated that the innate immune response may be delayed in adults infected with SARS-CoV-2. Farber commented: “If the innate response is really strong, that can reduce the viral load in the lungs, and the antibodies and T cells of the adaptive response have less to clear up.”
The team said it may also be possible that SARS-CoV-2 is less able to infect children’s cells, possibly because they express fewer proteins required by the virus to infect human cells.
The Columbia researchers are now testing these possibilities with cells from children versus adults.
The paper was published in Nature Immunology.
Related topics
Antibodies, Disease Research, Immunology, Vaccine
Related conditions
Acute Respiratory Distress Syndrome (ARDS), Children's multisystem inflammatory syndrome (MIS-C), Coronavirus, Covid-19
Related organisations
Columbia University Vagelos College of Physicians and Surgeons
Related people
Dr Donna Farber, Dr Matteo Porotto





Few studies show that pH decreases with age between 17 and 80 year old. Knowing that Coronovirus need low pH for a fusion with a cell it is possible to suggest that it could be one of reason why children have mild symptoms of COVID 19 and less likely to get infected.