Gene therapy boosts CAR-T power against glioblastoma
Posted: 14 July 2025 | Drug Target Review | No comments yet
Researchers at SR-TIGET in Milan have developed a novel gene therapy approach that supercharges CAR-T cell therapy against glioblastoma – strengthening treatment against one of the world’s deadliest brain cancers.
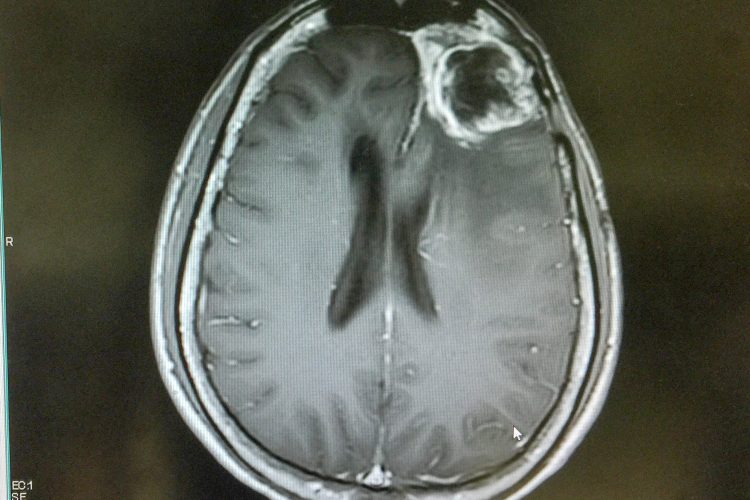
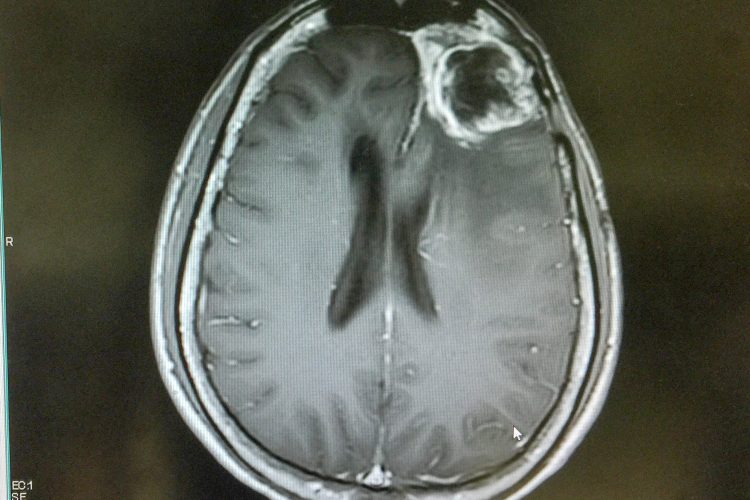
A team of researchers from the San Raffaele-Telethon Institute for Gene Therapy (SR-TIGET, Milan) have announced a novel gene therapy-based approach to bolster chimeric antigen receptor (CAR) T cell therapy for glioblastoma – one of the most aggressive and treatment-resistant brain tumours. The study, led by Nadia Coltella and Luigi Naldini and published in Science Translational Medicine, demonstrates how localised immune stimulation within the tumour microenvironment (TME) not only restores CAR-T cell activity but also recruits the body’s broader immune system to fight the tumour.
Reprogramming the tumour environment
The strategy uses gene therapy to target immune-stimulating cytokines directly into the tumour, enabling a “private crosstalk” with CAR-T cells. This boosts CAR-T persistence, triggers wider immune activation and significantly delays tumour growth in preclinical glioblastoma models.
Solid tumours like glioblastoma have been notoriously difficult for CAR-T cells to penetrate and control
“Solid tumours like glioblastoma have been notoriously difficult for CAR-T cells to penetrate and control,” explains Dr Frederico Rossari, first author of the study. “By reprogramming a population of tumour-infiltrating macrophages to deliver cytokines directly into the tumour, we’ve morphed the immunosuppressive TME into one supportive of immune cells, thus allowing CAR T cells to better persist, become activated and attack tumour cells.”
Building on prior innovation
This work expands on a gene therapy platform previously developed in the Naldini laboratory, which engineers hematopoietic progenitors to produce tumour-infiltrating macrophages capable of releasing immune-stimulating payloads. That approach has already reached first-in-human clinical testing as a stand-alone glioblastoma treatment under Genenta Science.
Two-pronged cytokine strategy
The SR-TIGET team engineered the macrophages to selectively release two cytokines within the tumour: interferon-α (IFN-α) and a modified version of interleukin-2 (IL-2). The former is known for enhancing immune activation and countering local suppression and the latter activates engineered CAR-T cells – leaving healthy tissue untouched.
“The private ‘crosstalk’ between genetically engineered macrophages and CAR T cells established in the TME ensures that the immune stimulants act only where needed, sparing the rest of the body from systemic toxicity, and specifically on the relevant target cells involved in the tumour attack, again preventing collateral damage and aberrant effects,” says Dr Giorgia Alvisi, co-first author of the study.
Transformative results in preclinical models
When tested in a mouse model that closely mimics human glioblastoma, this dual-cytokine approach overcame the typical inefficacy of CAR-T therapy in solid tumours. Tumour growth was slowed, survival extended and immune responses broadened.
“We observed not only reactivation of the CAR-T cells but also the recruitment of the host’s own T cells against a wider range of tumour antigens,” says Dr Nadia Coltella, senior co-corresponding author. “This phenomenon, known as antigenic spreading, was mostly dependent on IFN-α activity in the TME and is a key feature for creating effective immunity as it may overcome immune evasion by tumours targeted only through a single antigen by the CAR-T cells.”
Toward a future combination therapy
Dr Luigi Naldini, Director of SR-TIGET and Professor at Università Vita-Salute San Raffaele, emphasised the translational potential of the findings.
“This work represents another important step forward in our decade-long commitment to develop a novel gene and cell therapy strategy effective against tumours, as we have been able to do for several genetic diseases along the life of our institute.”
This work represents another important step forward in our decade-long commitment to develop a novel gene and cell therapy strategy effective against tumours
He adds that the Temferon trial, led by Genenta Science and already underway, is testing tumour-targeted IFN-α delivery as a stand-alone treatment in early-stage patients. The data so far has shown feasibility, safety, immune reprogramming and “early but promising indication of therapeutic benefit.” Looking ahead, combining Temferon with CAR-T therapy could “further enhance the benefit of the treatment and broaden its efficacy to a larger fraction of patients.”
Related topics
Cancer research, Cell Therapy, Central Nervous System (CNS), Chimeric Antigen Receptors (CARs), Cytokines, Gene Therapy, Immunotherapy, In Vivo, Oncology, Translational Science
Related conditions
Cancer, Glioblastoma
Related organisations
Genenta Science, the San Raffaele-Telethon Institute for Gene Therapy (SR-TIGET Milan)
Related people
Dr Frederico Rossari (Postdoc Fellow Targeted Cancer Gene Therapy Unit), Dr Giorgia Alvisi (Postdoc Fellow Targeted Cancer Gene Therapy Unit), Dr Luigi Naldini (Director of SR-TIGET and Professor at Università Vita-Salute San Raffaele), Dr Nadia Coltella (Research Associate Targeted Cancer Gene Therapy Unit)