Lupus reimagined: targeting the cause, not just the symptoms
Posted: 14 August 2025 | Drug Target Review | No comments yet
Engineered cell therapies are offering a potential new way to treat lupus – not by suppressing symptoms, but by reprogramming the immune system itself. For the first time, lasting remission looks like a real possibility.
Lupus is one of the most challenging autoimmune diseases to diagnose, treat and manage. Affecting millions of people worldwide – most commonly women between the ages of 15 and 45 – it occurs when the immune system mistakenly attacks the body’s own tissues. The result is widespread inflammation and potential damage to vital organs. Symptoms can include severe pain, rash, and fever. Until recently, treatment has largely focused on controlling symptoms, but the rise in engineered cell therapies has prompted researchers to explore new ways to restore immune balance, offering patients the possibility of lasting remission.
In conversation with Maya Bader, PhD, Director of Research at the Lupus Research Alliance (LRA), and Jennifer Meriwether, Director of Clinical Operations at Lupus Therapeutics, the clinical affiliate of the Lupus Research Alliance, we explored the science, strategy and potential of this groundbreaking area of research.
The promise of engineered cell therapies
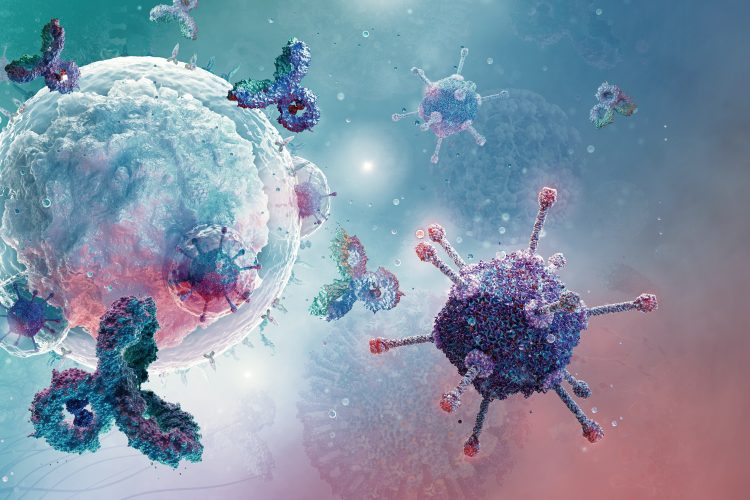
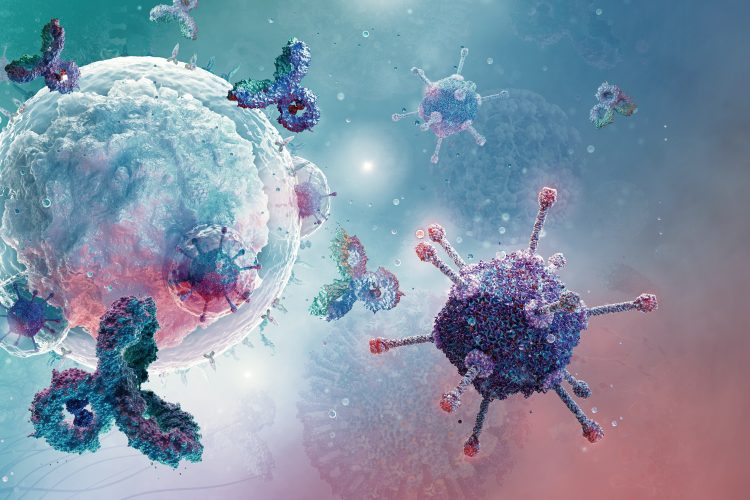
The premise of engineered cell therapy is both innovative and personalised. One method involves taking immune cells from a lupus patient, genetically modifying them to target and eliminate the disease-causing immune cells, and then reintroducing the reprogrammed cells with the goal of resetting the immune system.
Automation now plays a central role in discovery. From self-driving laboratories to real-time bioprocessing
This report explores how data-driven systems improve reproducibility, speed decisions and make scale achievable across research and development.
Inside the report:
- Advance discovery through miniaturised, high-throughput and animal-free systems
- Integrate AI, robotics and analytics to speed decision-making
- Streamline cell therapy and bioprocess QC for scale and compliance
- And more!
This report unlocks perspectives that show how automation is changing the scale and quality of discovery. The result is faster insight, stronger data and better science – access your free copy today
The promise here is that you’re potentially resetting the immune system back to a more ‘normal’ state.
“The promise here is that you’re potentially resetting the immune system back to a more ‘normal’ state.” says Dr Bader.
This marks a substantial shift from merely suppressing symptoms to addressing the disease at its root. Where current treatments rely heavily on long-term immunosuppressants like steroids – often accompanied by severe side effects – engineered cell therapies aim for longer remission periods or potentially even a cure.
Ms Meriwether adds, “the prospect of patients needing fewer medications – or experiencing longer periods without symptoms – would be an ideal outcome.”
A strategic leap: how the TRP-ECT programme came to life
The Lupus Research Alliance has played a key role in advancing lupus treatment by strategically investing in cell therapy research from its earliest stages.
Back in 2014, the Lupus Research Alliance funded the first proof-of-principle study demonstrating the potential of engineered cell therapies in lupus, awarding a grant to Dr Marko Radic at the University of Tennessee. That early-stage research would later prove pivotal. In 2024, the Lupus Research Alliance Lupus Insight Prize was awarded to Dr Radic and to Dr Georg Schett, whose team went on to lead the first successful clinical trials of engineered cell therapies in lupus patients. Dr Schett credited the foundational work funded by the Lupus Research Alliance as a key factor in the success of those investigational human studies. One of its most significant initiatives, the Targeted Research Program in Engineered Cell Therapies for Lupus (TRP-ECT), reflects over a decade of focused planning and long-term commitment to immune-resetting approaches.
The TRP-ECT programme – launched as part of the Lupus Research Alliance’s 2024 research strategy – builds on that foundation with the intent on expanding research on engineered cell therapies and the immune resetting concept as a whole. In the inaugural year, the Lupus Research Alliance awarded $4.1 million across 11 research projects, a significant investment, with continuing investments planned. The initiative focuses not only on advancing the science of immune-resetting therapies, but also on addressing the key unknowns: how to measure and assess long-term immune reprogramming and how to make these treatments safer and more accessible.


Lupus is a systemic autoimmune disorder characterised by immune dysregulation and chronic inflammation, which can affect the skin, joints, kidneys and other organs. One of its hallmark symptoms is a malar rash, often presenting in a butterfly-shaped pattern across the face. Image credit: © TarikVision / Shutterstock.com
From CAR T to Tregs
Much of the early excitement surrounding engineered cell therapies in lupus stemmed from CD19-directed CAR-T cells, which target and eliminate B cells, which drive the autoimmune response in lupus. But the field is rapidly evolving.
There’s now an explosion of different varieties of engineered cell therapies.
“There’s now an explosion of different varieties of engineered cell therapies,” explains Dr Bader. These include other types of engineered cells such as regulatory T cells (Tregs), engineered to restore immune tolerance, and alternate targets aimed at more precise elimination of harmful cell types rather than entire immune cell populations.
One project funded by the program uses a “fine-tuned strategy” to target OX40L, a protein involved in immune dysregulation and inflammation in lupus. Instead of eliminating all immune cells, you’re targeting a crucial driver of immune dysregulation and restoring immune balance, Dr Bader explained.
Put simply, this could lead to treatments that are more targeted, with fewer side effects for patients compared to the current iteration of cell therapies.
Clinical readiness: tackling challenges head-on
Despite the excitement, translating engineered cell therapies from preclinical promise to patient-ready treatment is not without obstacles. “These therapies are complicated, expensive and multifaceted,” Dr Bader said. “It’s the same kinds of translational issues we see elsewhere, but they’re significantly magnified here.”
The treatment requires significant time, follow-up and resource commitment – not just from clinical sites, but from patients and their families as well.
From a clinical operations standpoint, Ms Meriwether elaborates on the practical challenges: “The treatment requires significant time, follow-up and resource commitment – not just from clinical sites, but from patients and their families as well.”
Eligibility criteria for current trials remain stringent, and follow-ups are robust to ensure safety. “As it currently sits, the cost for these treatments is foreseeably high,” Ms Merriwether notes. “The preparation, delivery and monitoring all demand considerable physical resources and staff time. If these therapies prove effective, demand will rise – and both patients and health systems will need scalable ways to support them.”
Supporting safety, equity and scalability
The Lupus Research Alliance and Lupus Therapeutics are both working to ensure these therapies are safe, inclusive and accessible. Lupus Therapeutics plays a vital role in translating scientific discoveries into real-world treatments through close collaboration across research and care.
Lupus Therapeutics also supports numerous clinical trials through its Lupus Clinical Investigators Network (LuCIN) – comprised of over 60 research sites across North America. Beyond operational oversight, they run patient and physician education initiatives to help bridge the knowledge gap.
“Lupus Therapeutics hosted several webinars over the past two years focused on cell therapy implementation – informing and educating both patients and physicians – and have convened physician discussion forums as well,” says Meriwether. “Lupus Therapeutics also oversees a dedicated advisory group on cell therapy and recently included it as a key topic at the LuCIN Community annual meeting to address operational and site-level considerations.”
This kind of groundwork is essential. Breakthrough science only becomes breakthrough treatment when the people delivering it – clinicians, trial sites and patients – understand how to use it, what to expect and how to access it. By closing those gaps early, Lupus Therapeutics is helping to build the infrastructure these therapies will need to succeed in the real world.
Meanwhile, the Lupus Research Alliance’s research team is also leading efforts through the Accelerating Breakthrough Consortium (Lupus ABC) – a public–private partnership with the US Food and Drug Administration (FDA) aimed at expediting the development of new therapies for lupus. Within this initiative, a dedicated working group is focused specifically on engineered cell therapies. As Dr Bader explains, their first project aims to develop considerations for conducting CAR-T trials in lupus. The group brings together stakeholders with a range of perspectives to shape this early guidance. Looking ahead, its next phase will continue tackling questions about engineered cell therapies and other immune-resetting therapies as the field continues to progress.
Why lasting remission is finally within reach
Both Dr Bader and Ms Meriwether remain optimistic about the next steps.
He successfully showed the potential of this approach – disease-free remission for almost four years without any additional treatments or side effects. That opens a real avenue for a cure.
Dr Bader reflects on the milestone achievement by Dr Schett’s team: “His initial findings successfully showed the potential of this approach – disease-free remission for almost four years without any additional treatments or major side effects. That opens a real avenue for a cure. However, the approach is still in its early stages, and much remains to be understood – which is why the Lupus Research Alliance is continuing to invest in further research and supporting activities.”
Ms Meriwether adds, “Lupus is a very complex and heterogeneous disease. Individuals experience a wide variety of symptoms that vary in severity and frequency and that affect many organ systems. The possibility of significant improvement across such a broad population is absolutely worthy of hope.”
As science progresses and clinical systems evolve, the dream of transforming lupus care – from symptom management to immune reprogramming – is possible. For patients, families and clinicians, this research signals something extraordinary: the very real prospect of long-term remission.
Meet the experts


Dr Maya Bader is Director of Research at the Lupus Research Alliance. She manages the Translational Bridge Award (TBA) and the Common Mechanisms in Autoimmunity Insight Award. She also oversees several research initiatives, including the Common Mechanism in Autoimmunity partnership, the development of a lupus biomarker roadmap and the Lupus Research Alliance’s data strategy.
Dr Bader has 12 years of research experience and 12 years in scientific grant administration and program management. She previously served as Program Manager at the CHDI Foundation (Los Angeles, CA), where she managed a diverse portfolio of academic and industry-led research collaborations, and philanthropic development of therapeutics and biomarkers for Huntington’s disease. Prior to joining the Lupus Research Alliance, she was Associate Director of Scientific Grants at the Pancreatic Cancer Action Network (Manhattan Beach, CA), overseeing the scientific and administrative aspects of the organisation’s grants programme. Dr Bader earned her PhD from Rockefeller University in genetics and cell biology and was a Helen Hay Whitney Fellow at UCLA, studying developmental neurobiology.


As Director of Clinical Operations at Lupus Therapeutics, Jennifer Meriwether leads efforts to strengthen the North American-based Lupus Clinical Investigators Network and develop strategies to support individual site needs. She works closely with clinical sites, pharmaceutical sponsors and research organisations to manage trials aimed at developing therapies that improve the lives of people living with lupus.
Ms Meriwether is a clinical research professional with over 20 years of experience conducting and managing trials across pharmaceutical and device development.
Related topics
Antibodies, Autoimmune disease, Cell Therapy, Chimeric Antigen Receptors (CARs), Clinical Trials, Drug Discovery, Drug Discovery Processes, Immunology, Immunotherapy, Translational Science
Related conditions
Lupus