The partnership changing the pace of radiopharmaceutical development
Posted: 3 December 2025 | Drug Target Review | No comments yet
A new collaboration between Crown Bioscience and Medicines Discovery Catapult is bringing advanced tumour models together with world-class imaging and radiochemistry to accelerate the development of next-generation radiopharmaceuticals.
The global radiopharmaceuticals sector is experiencing a period of unprecedented expansion. Once confined to specialist research centres, radiopharmaceuticals have become a key element of precision medicine, using targeted radioactive compounds to visualise and treat disease at the molecular level. This surge is being driven by rapid scientific and technological advances, coupled with strategic collaborations that accelerate translation from discovery to clinic.
One such collaboration – between Crown Bioscience and Medicines Discovery Catapult (MDC) – aims to transform how new radiopharmaceuticals are developed and validated. By integrating Crown Bioscience’s preclinical expertise with MDC’s radiochemistry and imaging capabilities, the two organisations have established an end-to-end preclinical platform intended to de-risk development and accelerate translation into the clinic.
The science behind the surge
Bryan Miller, Director of Scientific and Technical Operations at Crown Bioscience, notes that rapid progress in imaging, radiochemistry and molecular targeting is fuelling the sector’s expansion. “The rapid global growth of the radiopharmaceuticals sector is being fuelled by a series of scientific and technological advances that are transforming diagnostics and therapeutic radiopharmaceuticals,” he says.
The rapid global growth of the radiopharmaceuticals sector is being fuelled by a series of scientific and technological advances that are transforming diagnostics and therapeutic radiopharmaceuticals.
Breakthroughs in molecular imaging, targeted radionuclide therapy and radiochemistry have enabled scientists to label molecules with diagnostic or therapeutic isotopes more precisely than ever before. This capability allows for earlier detection of disease, as well as personalised treatment tailored to a patient’s unique biology.
Miller points to advances in isotope production that have improved the availability of key isotopes such as lutetium-177 and actinium-225, both of which can be used to deliver radiation directly to tumours. At the same time, improvements in the chemical “chelators” that bind isotopes to targeting molecules have made these treatments safer and more versatile, allowing a wider range of radioactive elements to be used effectively.
“Progress in preclinical models and imaging modalities, coupled with the rise of theranostics and digital tools such as AI-driven imaging analysis, is driving broader adoption worldwide,” he adds. These developments are not only advancing oncology but are also beginning to inform new approaches to therapy in neurology, cardiology and infectious disease.
Targeted precision for better outcomes
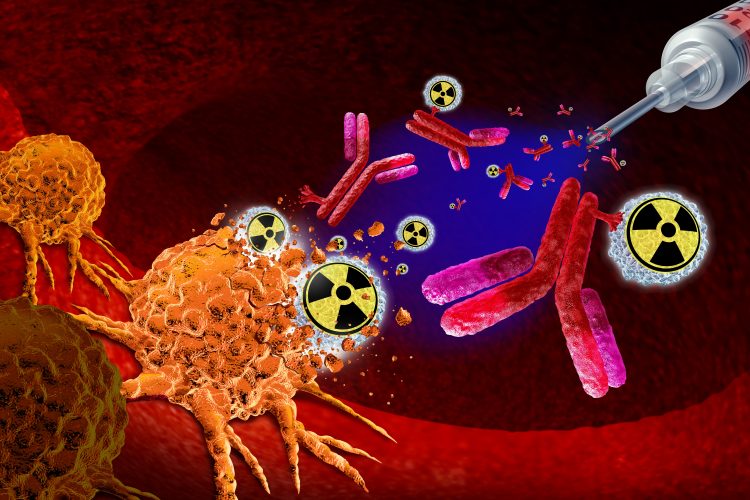
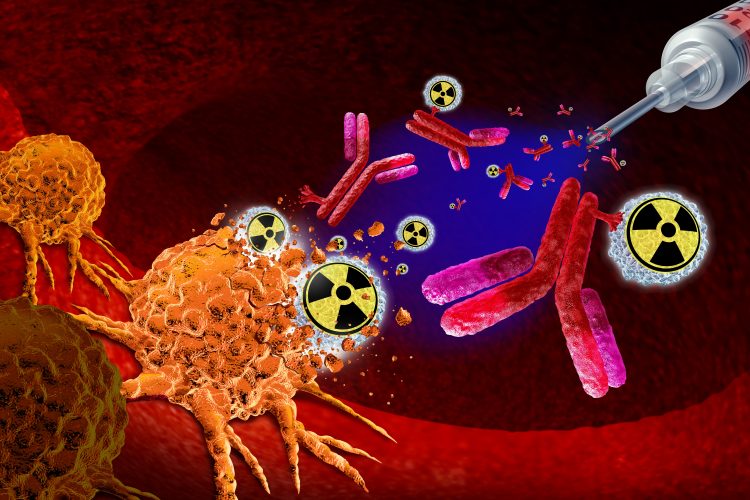
One of the greatest strengths of radiopharmaceuticals lies in their precision. Traditional cancer therapies such as chemotherapy or external beam radiation act broadly, often damaging healthy tissue alongside tumours. Radiopharmaceuticals, in contrast, use molecular targeting to deliver radioactive isotopes directly to diseased cells.
Radiopharmaceuticals achieve greater precision than traditional therapies by delivering radioactive isotopes directly to diseased tissues through highly specific molecular targeting, minimising exposure to healthy cells.
“Radiopharmaceuticals achieve greater precision than traditional therapies by delivering radioactive isotopes directly to diseased tissues through highly specific molecular targeting, minimising exposure to healthy cells,” Miller explains. By using targeting ligands – peptides, antibodies or small molecules that bind to tumour-specific markers – these agents provide selectivity unmatched by conventional treatments.
The result is twofold: improved diagnostic sensitivity and more localised therapy. “Clinicians can diagnose diseases more accurately, stage diseases with greater confidence and monitor therapeutic responses in real-time,” he says. For patients, the benefits are clear – personalised treatment, fewer side effects and, improved survival rates.
A collaborative model
The new platform jointly offered by Crown Bioscience and MDC brings together distinct but complementary expertise. Dr Juliana Maynard, Head of Translational Imaging at MDC, describes how the partnership provides an integrated translational biology platform .
Together, we have created a seamless pathway for companies developing radiopharmaceuticals, providing an integrated platform to take them from discovery through preclinical validation.
“This collaboration brings together Crown Bioscience’s collection of advanced in vitro and in vivo oncology models with MDC’s radiopharmaceuticals platform, which combines cutting-edge imaging technologies with world-class radiochemistry and translational expertise,” Dr Maynard explains. “Together, we have created a seamless pathway for companies developing radiopharmaceuticals, providing an integrated platform to take them from discovery through preclinical validation, and also into translational imaging studies.”
The collaboration allows developers to test compounds using clinically relevant tumour models, while simultaneously benefiting from MDC’s imaging and analytical infrastructure and expertise. This combination helps ensure that preclinical data more accurately predict human outcomes – a critical factor in reducing costly late-stage failures.
Translational models that mirror human biology
A major challenge in radiopharmaceutical development lies in predicting how a compound will behave once inside the human body. Crown Bioscience’s portfolio of patient-derived xenograft (PDX) models, alongside cell-derived xenografts (CDX) and organoids, offers a powerful way to model tumour biology in a translationally relevant context.
“Crown Bioscience’s clinically relevant PDX models provide the most accurate prediction of radiopharmaceutical behaviour by maintaining the genetic, histological and microenvironmental complexity of human tumours,” says Miller. These models enable precise assessment of biodistribution, targeting and therapeutic response.
Complementing the PDX portfolio, CDX models deliver reproducibility and scalability for comparative studies, while organoid systems allow scientists to probe tumour-specific mechanisms in vitro. “Together, these platforms generate translationally relevant data that more reliably anticipate clinical performance, supporting improved dosing strategies, safety evaluation and patient selection,” he adds.
De-risking development and accelerating translation
Radiopharmaceutical discovery and development remain high-risk endeavours, requiring not only technical sophistication, due to the nature of the medicines, but also substantial investment – as with all drug development. The integrated platform from Crown Bioscience and MDC aims to mitigate these challenges by reducing uncertainty and enhancing decision-making throughout the pipeline.
It not only helps innovators develop radiopharmaceuticals more efficiently but also provides them with the tools to de-risk their assets for investment, accelerate their journey to the clinic and ultimately improve patient outcomes.
By combining validated biological models with advanced imaging, researchers can identify safety issues early, optimise dose selection and confirm mechanisms of action before human trials begin. This approach lowers the likelihood of late-stage attrition, enabling researchers to make evidence-based decisions and focus resources on the most promising candidates.
“It not only helps innovators develop radiopharmaceuticals more efficiently but also provides them with the tools to de-risk their assets for investment, accelerate their journey to the clinic and ultimately improve patient outcomes,” Miller explains.
The collaboration also helps to create new opportunities for small and mid-sized biotechs that may lack access to specialist preclinical infrastructure. With both organisations providing end-to-end preclinical support, developers can progress more rapidly from discovery to proof-of-concept.
Expanding beyond oncology
Although oncology remains the most active area of radiopharmaceutical research, Miller notes that the field’s reach is broadening quickly. “Beyond oncology, radiopharmaceutical applications show strong promise in neurology, cardiology and infectious diseases,” he says.
In neurology, targeted radiotracers are advancing early detection of neurodegenerative diseases such as Alzheimer’s and Parkinson’s. In cardiology, new agents are improving the assessment of myocardial perfusion and receptor expression, guiding precision therapies for heart disease. Meanwhile, in infectious disease, molecular imaging is emerging as a tool for rapid, non-invasive localisation and monitoring of infection.
This diversification reflects a wider trend in medicine towards functional imaging and molecular diagnostics – areas in which radiopharmaceuticals are uniquely positioned to excel.
A strategic partnership for the next generation
Dr Maynard emphasises that the collaboration between Crown Bioscience and MDC is not only about technological integration but also about establishing a sustainable model for future innovation.
Using the correct tumour model is crucial in preclinical oncology radiopharmaceutical development.
“Using the correct tumour model is crucial in preclinical oncology radiopharmaceutical development,” she explains. “By enabling access to Crown Bioscience’s extensive library of well-characterised PDX models, alongside MDC’s radiochemistry and translational imaging platforms, we are supporting companies with the development, characterisation and clinical readiness of novel radiopharmaceutical agents.”
In practical terms, this means that companies can approach the partnership with a molecule at the discovery stage and progress through preclinical validation within a single collaborative framework. Such streamlining is expected to shorten development timelines and improve the reproducibility of translational data – both vital for maintaining competitiveness in an increasingly crowded field.
Personalised therapy
As radiopharmaceutical research continues to evolve, the partnership between Crown Bioscience and MDC demonstrates how integrating robust tumour models with advanced imaging and radiochemistry can streamline discovery, reduce risk and accelerate the delivery of targeted therapies to patients.
Meet the experts
Bryan Miller, Director of Scientific and Technical Operations at Crown Bioscience


Dr Juliana Maynard, Head of Translational Imaging at Medicines Discovery Catapult


Juliana began her career at the University of Manchester before joining AstraZeneca. From there, she recognised the potential of medical imaging to enhance and accelerate drug discovery and established a commercial imaging service designed to make these resources easily accessible to the UK drug discovery community.
In 2019, she joined Medicines Discovery Catapult as the Head of Translational Imaging. In this role, Juliana leads a multidisciplinary team that supports drug discovery innovators by validating therapeutic targets and platforms for clinical use, ultimately helping to bring more medicines to patients faster.
Related topics
Drug Development, Drug Discovery, Oncology, Organoids, Precision Medicine
Related conditions
Cancer, Infectious diseases, Neurodegenerative diseases
Related organisations
Crown Bioscience, Medicines Discovery Catapult (MDC)