A T cell receptor immunotherapy against a novel target
Posted: 7 June 2024 | Ana Pereira Ribeiro (Immunocore), Drug Target Review | No comments yet
In this Q&A, Associate Director, Research at Immunocore, Dr Ana Pereira Ribeiro, talks about IMC-R117C, a T cell receptor bispecific immunotherapy directed towards a novel target, PIWIL1, and about to enter Phase I testing in colorectal and gastrointestinal cancers.
How does Immunocore’s TCR technology differentiate itself from other approaches to targeted cancer therapy?
Our proprietary ImmTAC (Immune Mobilizing Monoclonal TCRs Against Cancer) technology is comprised of a bispecific molecule where the effector end (anti-CD3) is designed to specifically activate the immune system (ie, T cells) against tumour cells to destroy them. A key difference from existing immunotherapies is that the ImmTAC platform can access intracellular targets, as these are processed and presented by the tumour cell and recognised by the T cell receptor (TCR) that represents the targeting end of the platform.
While currently available antibody-based cancer therapies can only bind to proteins accessible on the cancer cell surface (<10 percent of the human proteome), the ImmTAC platform can access intracellular proteins, which represent around 90 percent of the proteome, allowing us to target novel cancer antigens, such as PIWIL1, the target for IMC-R117C.
Can you explain the mechanism of action by which ImmTAC molecules selectively target and kill cancer cells?
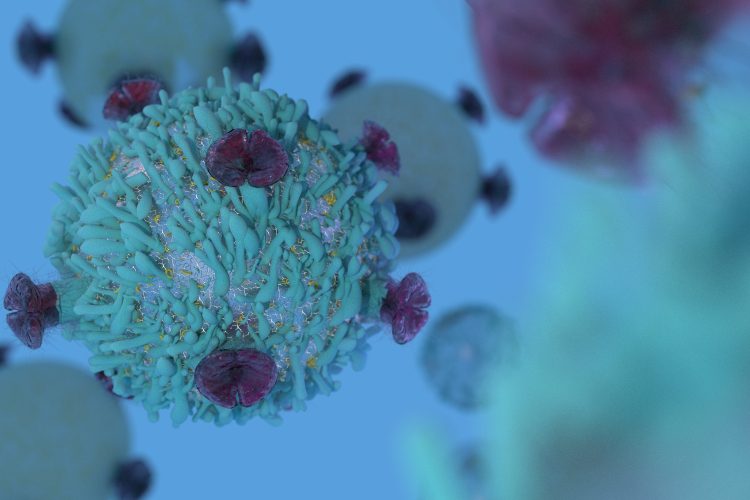
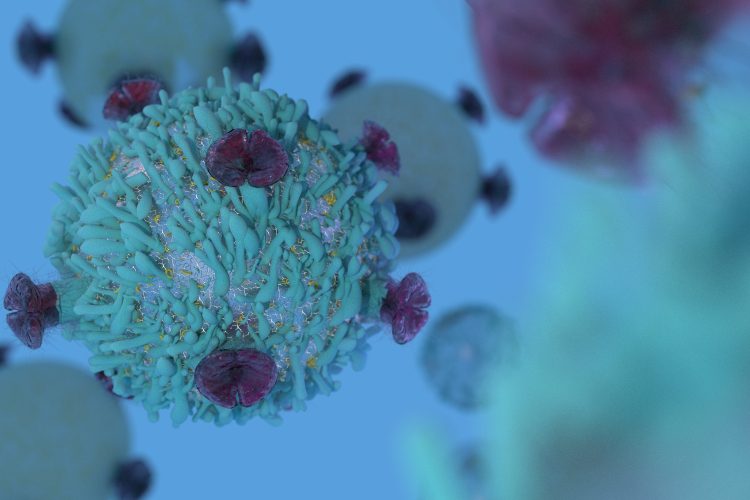
As represented by our launch of the world’s first TCR therapy in 2022, ImmTAC molecules are designed to recognise and bind to their chosen target antigen when presented as a peptide in the context of an HLA molecule (ie, peptide/HLA complex) on the surface of the tumour cell. The ImmTAC molecule is able to target the peptide/HLA complex through an affinity enhanced TCR domain, which is capable of recognising even very low numbers (ie, two to 10) of peptide/HLA targets on the tumour cell. Once bound to the tumour cell, the effector domain (an anti-CD3) of the ImmTAC is capable of redirecting polyclonal T cells to kill the cancer cell through lytic processes. In this way, the ImmTAC molecule forms a bridge between the cancer cell and the T cell, bypassing the need for the patient’s T cells to recognise the tumour specifically.
What advantages does Immunocore’s approach offer in treating both haematologic and solid tumours, particularly those considered “cold” tumours with low mutation rates?
As discussed, the ability of our ImmTAC platform to unlock a broad range of intracellular targets, normally not accessible by antibody-based cancer therapies, opens up opportunities to treat a range of tumours of different origin. Unlike existing immunotherapies that are designed to “remove the brakes” from exhausted, pre-existing tumour-specific T cells, the ImmTAC platform can redirect any T cell in the patient’s body to recognise and kill tumour cells expressing the target of interest the ImmTAC was engineered for.
Due to this unique mechanism that does not rely on pre-existing immunity, the ImmTAC platform can be used to treat “cold” tumours normally associated with low mutation rates and minimal baseline immune infiltration. The proof for this came with the approval of KIMMTRAK (tebentafusp-tebn) by the FDA in 2022 for the treatment of HLA-A*02:01+ metastatic or unresectable uveal melanoma, a historically “cold” tumour known to be resistant to current available checkpoint immunotherapies. Tebentafusp was shown to increase T cell recruitment into tumours that typically have poor immune infiltration, providing novel benefit where checkpoint inhibitors have demonstrated limited efficacy.
What preclinical evidence supports the efficacy and safety of IMC-R117C as a potential treatment for colorectal and gastrointestinal cancers?
To support IMC-R117C’s clinical trial application, extensive in vitro analyses were performed to characterise the pharmacologic activity of the molecule and assess any potential toxicity. Overall, IMC-R117C demonstrated desired specificity for redirecting T cells against the target antigen over-expressed in colorectal and gastric cancer cell lines. Additionally, the possibility of cross-reactivity with normal human tissues and the potential for any organ-specific toxicities associated with the molecule were tested through in vitro functional assays and predictive molecular cross-reactivity studies. Once enrolling, the Phase I trial of IMC-R117C will follow a dose escalation protocol in order to establish a safe and efficacious dosing regimen.
In terms of the anti-CD3 immune-activating effector function, how does Immunocore ensure the balance between efficacy against cancer cells and minimising off-target effects on healthy tissues?
Our ImmTAC molecules are engineered to specifically recognise the target antigen, with that specificity being extensively studied in molecular and functional assays. Whereas the TCR arm of the ImmTAC is engineered to very high affinity (picomolar range), the anti-CD3 effector binds to CD3 in T cells with lower affinity (nanomolar), which makes it active only when there is strong engagement of the TCR in the presence of the correct antigen. In the absence of the target antigen, the anti-CD3 binds weakly to T cells; therefore, there is very low risk of off-target T cell binding leading to their engagement and function.
How does Immunocore plan to leverage the ImmTAC platform in future clinical trials beyond colorectal and gastrointestinal cancers?
Built on our proprietary ImmTAX (Immune Mobilizing Monoclonal TCRs Against X disease) platform, Immunocore has a diverse portfolio of bispecific therapies across three disease areas (cancer, infectious and autoimmune diseases). We also continue to advance our industry-leading discovery platform, spanning from target validation to TCR engineering, to validate more novel targets beyond PIWIL1 and develop the next generation of targeted immunotherapies to benefit more patients in indications of unmet need.
About the author


Dr Ribeiro is an Associate Director in Pipeline Biology at Immunocore, leading a team responsible for the generation of preclinical efficacy and safety data from early stages of drug screening up to candidate nomination and follow up IND/CTA-enabling studies. She has deep knowledge in Immunology and T cell biology, and 13 years of experience in Research (seven of them in biotech at Immunocore), including pipeline programme leadership. Dr Ribeiro holds a PhD in Biomedical Sciences from University of Porto, Portugal, studying T cell and thymus development.
Related topics
Cancer research, Clinical Trials, Drug Development, Drug Targets, Immunotherapy, T cells
Related conditions
Cancer Research, Colorectal cancer, gastrointestinal cancer
Related organisations
Immunocore
Related people
Dr Ana Pereira Ribeiro (Immunocore)