Targeting GLP-1 in the brain could transform obesity care
Posted: 2 June 2025 | Drug Target Review | No comments yet
What if a single hormone could control appetite in two entirely different ways? Professor Stefan Trapp of University College London reveals how GLP-1’s dual role in the brain and gut could transform obesity treatment.
For decades, researchers have explored how our bodies regulate hunger and satiety. A central player in this system is glucagon-like peptide 1 (GLP-1), a hormone originally known for its role in regulating blood sugar. But as Professor Stefan Trapp, an expert in autonomic neuroscience and metabolic disease at University College London, explains, GLP-1’s role in appetite is far more complex – with two distinct sources (gut and brain) acting through very different mechanisms.
With nearly 20 years of experience investigating how the brain controls eating behaviour, Trapp’s research has helped shift the scientific narrative. His groundbreaking work on preproglucagon (PPG) neurons, and on the blood–brain barrier’s role in limiting GLP-1’s access to the brain, is redefining how we think about obesity, appetite, and drug development.
The gut-brain axis: challenging the old GLP-1 model
The original theory was simple: food enters the gut → the gut releases GLP-1 → GLP-1 travels via the bloodstream into the brain → GLP-1 induces more GLP-1 release within the brain → appetite is suppressed.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
But Trapp’s lab discovered a critical flaw: preproglucagon (PPG) neurons, which produce GLP-1 in the brainstem, lack receptors for circulating GLP-1. This means the gut-derived hormone GLP-1 cannot directly stimulate these brain cells. Instead, the central GLP-1 system operates independently, driven by physiological signals such as gastric distension and neural inputs, rather than circulating GLP-1.
GLP-1: one molecule, two modes of action
| Peripheral GLP-1 | Central GLP-1 |
| Acts as a hormone | Acts as a neurotransmitter |
| Circulates via bloodstream | Released at specific brain synapses |
| Regulates blood sugar | Regulates appetite |
| Widespread, non-specific receptor activation | Spatially precise, localised signalling |
This discovery prompted a deeper investigation into the separate roles of peripheral and central GLP-1. Trapp highlights the fundamental differences between hormonal and neurotransmitter action. “A neurotransmitter,” he explains, “is released within the brain at a very specific site. It acts there at specific synapses and just covers a small space, and it therefore produces temporally and spatially very precise signalling”.
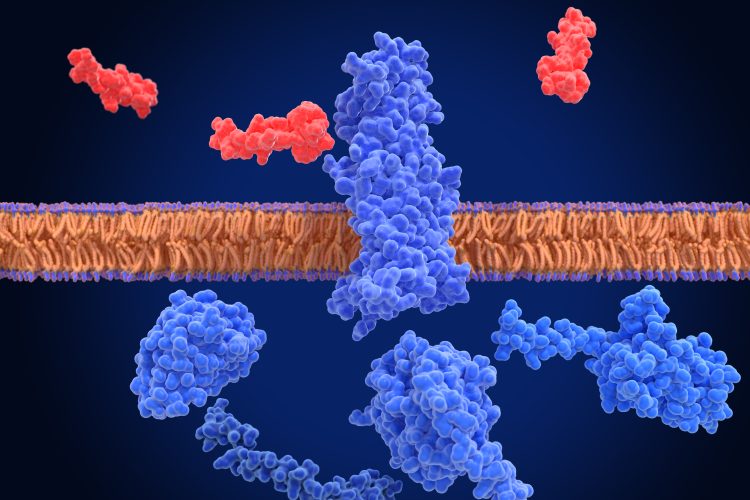
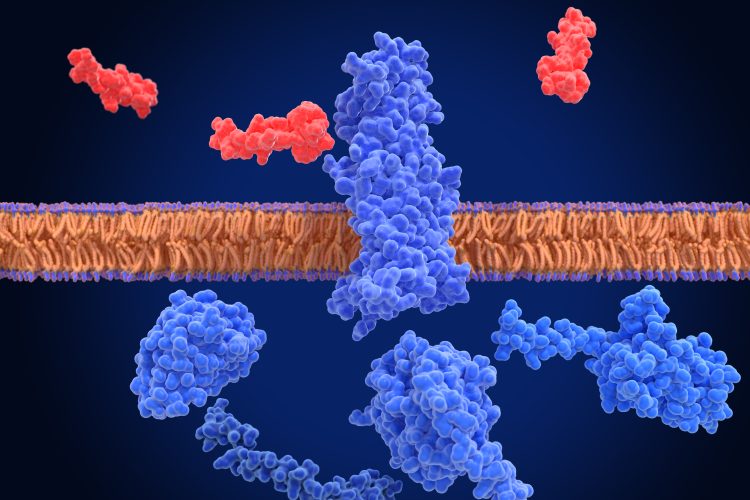
Peptides like GLP-1 struggle to cross this barrier, challenging assumptions that peripheral GLP-1 can easily impact brain function.
Peripheral GLP-1 acts as a hormone, released into the bloodstream after a meal, and is capable of reaching any GLP-1 receptor throughout the body simultaneously for more widespread actions. Its primary role is in enhancing insulin release in response to rising blood sugar levels, a mechanism exploited in type 2 diabetes treatments. In contrast, GLP-1 produced within the brain acts as a neurotransmitter. It is released at specific synaptic sites within the brain, exerting spatially precise signalling. This means that GLP-1 can be released in one brain region, like the hypothalamus, without necessarily affecting another, such as the amygdala. This localised action allows for a fine-tuned regulation of different brain functions related to appetite.
Furthermore, Trapp emphasises the significant barrier between the bloodstream and the brain – the blood–brain barrier (BBB). “It keeps our brain safe from all sorts of substances, chemicals and bacteria,” Trapp says. Peptides like GLP-1 struggle to cross this barrier, challenging assumptions that peripheral GLP-1 can easily impact brain function. This protective mechanism, while crucial for brain health, presents a significant challenge for drug delivery, hindering the development of therapies that target central GLP-1 pathways.
This led Trapp’s team to explore whether GLP-1 systems in the brain and periphery might operate independently. Their findings increasingly support this idea, suggesting that effective therapy might require engaging both systems differently.
Evidence for separate roles
Several lines of evidence support the notion of distinct roles for peripheral and central GLP-1 in appetite regulation:
- Differential breakdown: Peripheral GLP-1 has a very short half-life in the blood (around two minutes) due to enzymatic degradation. While drugs used to treat diabetes inhibit this enzyme to prolong GLP-1 action on blood glucose, they do not translate to a significant effect on food intake.
- Targeting the brain directly: Experiments involving the direct injection of GLP-1 into the brain, or the selective activation of central GLP-1-producing neurons, have consistently shown a strong link between central GLP-1 action and reduced food intake.
- Combined effects: Reseach conducted in Professor Trapp’s lab has demonstrated that combining the activation of brain GLP-1 release with peripherally injected GLP-1 receptor agonists results in a greater reduction in food intake than either treatment alone. This suggests that they are acting on different sets of receptors.
- Limited brain penetration of agonists: Studies using fluorescently labelled GLP-1 receptor agonists like semaglutide and liraglutide have shown very limited penetration into most brain regions beyond the circumventricular organs – areas where the blood–brain barrier is less effective and allows the brain to sample blood contents. These regions, such as the area postrema and median eminence, are designed to sample blood contents, enabling some access for substances that would otherwise be excluded. However, even with this limited access, most brain regions rich in GLP-1 receptors – particularly those involved in appetite regulation – showed minimal drug presence. This further supports the theory that the central and peripheral GLP-1 systems are not only anatomically but also functionally distinct.
Therapeutic advantages and challenges of targeting central GLP-1
The potential therapeutic benefits of targeting the brain’s GLP-1 system are significant. Trapp’s team’s animal studies have shown that stimulating central GLP-1 release can effectively suppress food intake. This provides a strong basis for developing therapies that more precisely modulate appetite control pathways within the brain. When asked about the therapeutic advantages of targeting the brain’s GLP-1 system, Trapp shares promising findings. “What we see from our ongoing experiments is that these GLP-1-producing cells in the brain have a clear ability to suppress food intake”.
What we see from our ongoing experiments is that these GLP-1-producing cells in the brain have a clear ability to suppress food intake.
Using advanced genetic tools, Trapp’s team can selectively stimulate GLP-1-producing neurons in animal models. The results? A strong, temporary reduction in food intake lasting around four hours. “But the GLP-1 drugs from the periphery, of course, are designed to have a long lifetime in the body,” Trapp explains, “which means they provide a more prolonged appetite-suppressing effect”.
So, while central stimulation shows promise, its effects are currently relatively short-lived. Developing drugs that can activate central GLP-1 pathways effectively – and for longer durations and ensuring they cross the blood–brain barrier remains a major challenge.
“We’re trying to figure out which are the GLP-1 receptor populations within the brain that are important for food intake, but that don’t produce side effects,” Trapp says. One of the most significant side effects of current GLP-1 receptor agonists like semaglutide is nausea – possibly linked to how and where these drugs act in the brain.
Despite this promise, considerable challenges remain – particularly the difficulty in delivering drugs across the blood–brain barrier to selectively activate central GLP-1 neurons. Current research in Professor Trapp’s lab, in collaboration with Dr Lora Heisler’s team in Aberdeen, is focused on identifying specific GLP-1 receptor populations in different brain regions and understanding their precise roles in regulating food intake and related behaviours. This work aims to pinpoint targets for future therapies that minimise side effects while enhancing efficacy.
The nausea conundrum
Professor Trapp also investigates the side effects associated with current GLP-1 receptor agonists, particularly nausea. Emerging evidence suggests that these drugs, due to their ability to access the circumventricular organs – such as the area postrema, a brain region involved in nausea responses – may trigger this adverse effect. This highlights a critical consideration in drug development: while enhancing brain penetrance might appear beneficial for targeting central appetite pathways, it could also exacerbate side effects.
To better understand the widespread effects of these agonists, Professor Trapp explains the use of c-Fos – a protein marker of neuronal activation. While studies have shown increased c-Fos activity throughout the brain following administration of GLP-1 receptor agonists, further investigation revealed that this activation often does not correlate with the presence of GLP-1 receptors in those same neurons. This suggests that the observed activation in many brain regions is indirect – likely triggered by the drug binding in more accessible areas, such as the circumventricular organs, which then transmit signals to other parts of the brain.
Future directions
Ongoing research continues to highlight the complexity of the GLP-1 system and the need for a more nuanced understanding of the distinct roles played by peripheral and central GLP-1. The future of therapeutic interventions for obesity may lie in developing strategies that selectively target specific GLP-1 receptor populations within the brain – potentially minimising side effects while maximising their impact on appetite regulation and related behaviours such as food reward.
As Professor Trapp’s work deepens our understanding of the communication between the gut and the brain – particularly in mapping the roles of different GLP-1 receptor populations in brain regions beyond basic satiety signals – we move closer to developing more effective, targeted treatments for obesity and metabolic disorders, including those that influence subconscious food cues and the motivational pathways associated with eating.
References
- Brierley DI, Holt MK, Singh A, de Araujo A, McDougle M, Vergara M, et al. Central and peripheral GLP-1 systems independently suppress eating. Nature Metabolism. 2021 Feb;3(2):258–73.
- Gabery S, Salinas CG, Paulsen SJ, Ahnfelt-Rønne J, Alanentalo T, Baquero AF, et al. Semaglutide lowers body weight in rodents via distributed neural pathways. JCI Insight. 2020 Mar 26;5(6).
- Huang KP, Acosta AA, Ghidewon MY, McKnight AD, Almeida MS, Nyema NT, et al. Dissociable hindbrain GLP1R circuits for satiety and aversion. Nature. 2024 Jul 10;632(8025):585–93.
Meet Professor Stefan Trapp


Related topics
Central Nervous System (CNS), Drug Discovery, Drug Discovery Processes, Hormones, Neurons, Obesity, Obesity
Related conditions
Metabolic disorders, Obesity, Type-2 diabetes
Related organisations
University College London
Related people
Professor Stefan Trapp (University College London)








