New developments in the research field of immuno-oncology
Posted: 30 April 2021 | Victoria Rees (Drug Target Review) | No comments yet
The exciting potential of immunotherapy for cancer treatment continues its exploration and here, Drug Target Review investigates three of the latest pre-clinical developments in immuno-oncology research.
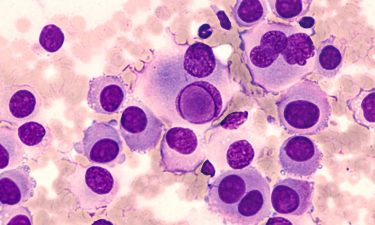
Research shows natural killer cells provide promise for immunotherapy
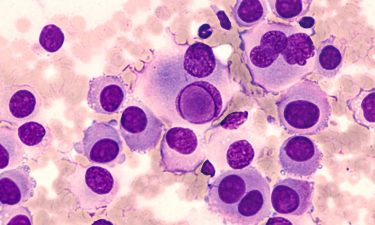
Scientists at McMaster University, Canada, have shown in new research that changing the metabolism of natural killer (NK) immune cells allows them to overcome the hostile conditions found inside tumours and destroy advanced ovarian and lung cancer.
“In this study, we discovered that the metabolism, or energy ‘hub’, of NK cells is paralysed by tumours, causing the NK cells to undergo an energy crisis and lose their tumour-killing functions,” said Sophie Poznanski, a PhD student and lead author of the study. “With that understanding, we were able to reverse the dysfunction of NK cells by repurposing a pre-existing metabolism drug that restored their energy production.”
Published in Cell Metabolism, the study shows that NK cells can also be modified to mimic the metabolism of tumours. These modified NK cells proved to be far better adapted for the hostile tumour environment, the team found.
“We were just hoping that the modified NK cells would better resist suppression in tumours. We were astounded to see that not only did they show no suppression, but they paradoxically functioned better inside of the tumour than outside of it,” said Poznanski.
“This is the first report of an antitumour immune cell that exploits the hostility of tumours for their own advantage,” said senior author Professor Ali Ashkar. “Generating cytotoxic immune cells to have tumour-like metabolism is key for their antitumour functions in a very hostile environment of a solid tumour. This could be a paradigm shift for immune cell-based cancer immunotherapy.”
So far, NK cells have only proven effective against blood cancers. However, re-programmed and trained NK cells could afford patients with otherwise terminal cancers with a safe and effective treatment option. Furthermore, immunotherapy with NK cells has already proven safe with few, if any, side effects.


Bispecific antibodies to target cancer
This research revealed a novel targeted immunotherapy approach that employs new antibodies against genetically altered proteins to target cancers. The technique was developed at the Johns Hopkins Kimmel Cancer Center, US.
The researchers targeted their immunotherapy approach to alterations in the common cancer-related p53 tumour suppressor gene, the RAS tumour-promoting oncogene or T-cell receptor genes. Their findings are reported in three related studies published in Science Immunology, Science and Science Translational Medicine.
Although common across cancer types, p53 mutations have thus far not been successfully targeted with drugs. Genetic alterations in tumour suppressor genes often result in their functional inactivation.
“Traditional drugs are aimed at inhibiting proteins. Inhibiting an already inactivated tumour suppressor gene protein in cancer cells, therefore, is not a feasible approach,” said Dr Emily Han-Chung Hsiue, lead author on the Science paper.
Instead of drugs, the researchers set out to target these gene alterations with antibodies. Conventional antibodies require an antigen target on the cell surface – most commonly a protein that looks like a foreign invader to the immune system. However, the proteins produced by mutant oncogenes and tumour suppressor genes are inside the cells, out of reach from conventional antibodies. However, proteins are routinely degraded within cells, generating protein fragments called peptides.
“These peptides can be presented on the cell surface when complexed with the human leukocyte antigen (HLA) proteins,” said Katharine Wright, postdoctoral fellow and a lead author on the Science Immunology paper. “Mutated proteins in cancer cells can also be degraded and generate mutant peptides presented by the HLA molecules. These mutant peptide HLA complexes serve as antigens and mark cancer cells as foreign to the immune system.”


They developed an approach in the form of bispecific antibodies, comprising one component that specifically recognises cancer cells and another component that recognises immune cells and brings both cells together. In laboratory and animal tumour cell models, it resulted in the destruction of tumour cells.
“This therapeutic strategy is dependent on a cancer containing at least one p53 or RAS alteration and the patient having an HLA type that will bind to the mutant peptide to present it on the cell surface,” said senior author Associate Professor Shibin Zhou, a study leader.
In the Science Translational Medicine paper, the researchers report that the powerful bispecific antibody approach they developed could also be used for the treatment of T-cell cancers. In animal models, the researchers showed that their approach selectively killed the cancerous T cells while sparing the majority of healthy T cells.
The scientists say the next research steps are to assess whether the strategy can be applied to other gene alterations in p53, KRAS and other cancer driver genes.
“We intend to develop a large number of bispecific antibodies that would target such genes,” said Alex Pearlman, PhD student and co-author of the three studies. “Although any individual bispecific antibody would target a small fraction of cancer patients, a suite of antibodies would allow for the treatment of many patients.”
Success of sequential treatment approaches with anti-PD-1 agents and targeted therapy
Researchers at Moffitt Cancer Center, US, have investigated how to combine and sequence new therapies to improve survival of patients with advanced melanoma. In a new article published in Cancer Immunology Research, the team demonstrated that sequential administration of immunotherapy followed by targeted therapy prolongs antitumour responses in pre-clinical models and may be a potential treatment option for patients.
One of the most common genetic alterations in melanoma are mutations of the BRAF gene, which affect approximately 50 percent of patients. These alterations result in downstream signalling through the protein MEK and stimulation of cell growth, invasion and survival. Several therapies that target both BRAF or MEK have been approved and standard treatment for patients who have BRAF mutations is now combination therapy with BRAF and MEK inhibitors.
Given the success of both BRAF/MEK inhibitors and immunotherapies, researchers have attempted to combine these two classes of anticancer therapies. However, some of these combinations have not always been successful.
“Initial attempts to develop targeted therapy/immunotherapy combinations clinically were not successful due to severe toxicity,” said Dr Keiran Smalley, lead researcher.
These toxicities led the research team to determine whether using a sequential treatment approach rather than a simultaneous combination approach would lead to durable antitumour activity in BRAF and NRAS-mutated melanoma.
The researchers analysed sequential combinations of immunotherapy followed by either BRAF/MEK-targeted therapy or another targeted therapy combination (ceritinib/trametinib) and vice versa in pre-clinical mouse models. They discovered that immunotherapy followed by targeted therapy was more effective than either treatment approach alone. While using targeted therapy followed by immunotherapy was better than targeted therapy alone, it was not as effective as the immunotherapy-targeted therapy sequence.
The team discovered the immunotherapy-targeted therapy sequence modulated the environment to promote immune cell functions resulting in antitumour activity while simultaneously blocking activity that permitted tumour cell escape from immune detection. They also showed that the immunotherapy-targeted therapy sequence enriched the melanoma cells for proteins that promoted immune cell detection and suppressed signalling pathways associated with drug resistance.
…sequential administration of immunotherapy followed by targeted therapy prolongs antitumour responses”
Results from this research suggest that sequential treatment approaches with anti-PD-1 agents followed by targeted therapy may be clinically beneficial and several ongoing trials are currently investigating this hypothesis.
“Together, our data demonstrates that sustained antitumour responses to targeted therapy are dependent upon a vigorous, sustained immune response and that upfront use of immunotherapy can augment this,” said Smalley.
Related topics
Drug Development, Immuno-oncology, Immunotherapy, Molecular Targets, Oncology
Related conditions
Cancer
Related organisations
Johns Hopkins Kimmel Cancer Center, McMaster University, Moffitt Cancer Center