Cell-derived therapy may help repair abnormal heart rhythm
Posted: 15 April 2022 | Ria Kakkad (Drug Target Review) | No comments yet
A new study has found vesicles secreted from human heart cells may repair damaged tissue and prevent lethal heart rhythm disorders.
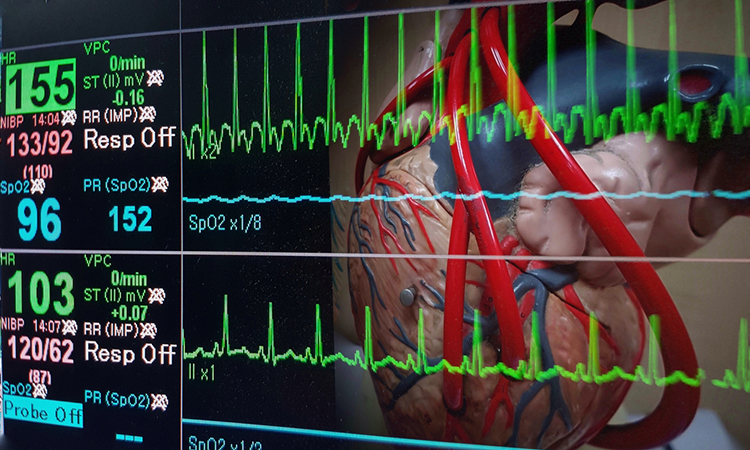
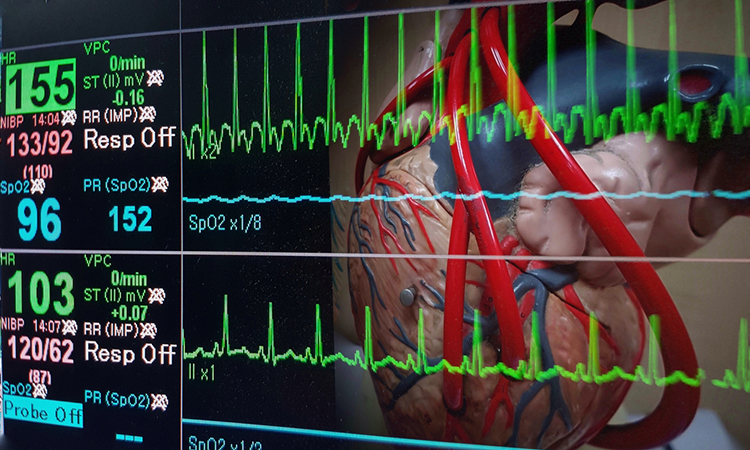
New research from the Smidt Heart Institute at Cedars-Sinai, US has found vesicles secreted from human heart cells may repair damaged tissue and prevent lethal heart rhythm disorders. The research, published in the European Heart Journal, could lead to a new way to treat a heart rhythm problem called ventricular arrhythmia—a top cause of sudden cardiac death.
Ventricular arrhythmias can occur after a heart attack damages tissue, causing chaotic electrical patterns in the heart’s lower chambers. This leads to the heart beating so rapidly that it cannot support the circulation, leading to a lack of blood flow and, if untreated, death. Current treatment options for ventricular arrhythmias caused by heart attacks are far from ideal. These include medications with major side effects, implanted devices to provide an internal shock, and a procedure called radiofrequency ablation in which parts of the heart are purposely destroyed to interrupt disruptive electrical signals. Recurrence rates are, unfortunately, high for all of these.
The researchers carried out their study in laboratory pigs that experienced a heart attack. They injected some of the laboratory pigs with tiny, balloon-like vesicles, called exosomes, produced by cardiosphere-derived cells (CDCs), which are progenitor cells derived from human heart tissue. Exosomes are hardy particles containing molecules and the molecular instructions to make various proteins, thus they are easier to handle and transfer than the parent cells, or CDCs. One group of pigs received an injection of CDC-derived exosomes in their hearts and the other a placebo.
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
“The exosomes reduced the amount of scar tissue formed in the injured regions of the heart, normalising the rhythm without weakening the heart,” said Dr Eduardo Marbán, a co-author on the study.
Related topics
Targets, Therapeutics
Related conditions
heart attacks, Ventricular arrhythmias
Related organisations
Smidt Heart Institute at Cedars-Sinai
Related people
Dr Eduardo Marbán