New biomarker advances cancer treatments
Posted: 27 October 2023 | Drug Target Review | No comments yet
Researchers have discovered ways to enhance NIR-PIT to ensure tumours are treated sufficiently and improve patient outcomes.
A biomarker based on microbubbles has been used to evaluate the success of near-infrared photoimmunotherapy (NIR-PIT) by scientists at Nagoya University in Japan and their collaborators. Tracking the microbubbles with ultrasound, the team identified areas where cancer therapy had not been fully applied. Their findings propose ways to improve NIR-PIT and make it a feasible alternative treatment for various types of cancer.
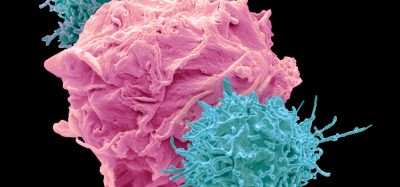
NIR-PIT combines the use of antibodies and near-infrared light to selectively destroy cancer cells while preserving healthy tissues. The antibody targets and binds to cancer cell proteins, creating a light-absorbing substance called IR700. IR700 activates and releases energy when it is exposed to near-infrared light, which destroys cancer cells. Along with surgery, radiation, chemotherapy and cancer immunotherapy, NIR-PIT is considered the fifth cancer treatment.
Physicians need to determine the optimum level of light intensity to destroy abnormal cell growth while also avoiding damage to healthy cells, to effectively treat a tumour. However, it is challenging to ensure uniform irradiation of target cells during surgery because the host tissue reflects and scatters light. To prevent undertreating the whole tumour with insufficient light irradiation, physicians require an indicator to decide its effectiveness.
Dr Kazuhide Sato of Nagoya University Graduate School of Medicine and his collaborators studied differences in tumour vessels compared to host cells. Previous studies have informed scientists that tumour vessels have irregular shapes, gaps between cells, and poor drainage. Poor drainage during NIR-PIT treatment helps therapeutic nanoparticles reside in the tumour and then enter cancerous tissue, resulting in a therapeutic effect known as the enhanced permeability and retention (EPR) effect.
NIR-PIT treatment causes rapid tumour cell death which increases permeability in the tumour vessels and leads to a ‘super EPR effect’ (SUPR). The SUPR effect is 24-times higher than other therapies. It is likely that the treatment has been successful if the SUPR effect occurs all over the tumour. If it is isolated to particular regions, it is less likely that the treatment has been successful.
To evaluate the success of the treatment, the team used the increased permeability to test whether larger fluorescent nanoparticles, like Sonazoid microbubbles, could be retained. Microbubbles provide an easy way to measure the SUPR effect as they can be clearly detected by reflecting harmonic signals off them.
“We investigated with larger-sized fluorescent particles of two millimetre and five millimetre sizes”, said Dr Sato. “We found that retention increased with both sizes.” The team used ultrasound imaging to track microbubbles, creating a new biomarker that measured the SUPR effect before and after treatment and evaluated the effectiveness of NIR-PIT. Dr Sato explained: “In short, the higher the retention, the higher the anti-tumour effect of NIR-PIT.”
Dr Sato hopes that this discovery will advance cancer patient treatment. “Using this new concept, we could confirm and predict the effects of the treatment after NIR light irradiation,” he stated. “This is especially important for patients who receive insufficient treatment. Additional irradiation could be performed flexibly. Since ultrasound imaging equipment has already been introduced in most hospitals and the microbubble contrast agent used in this study has already been approved, this technology is easy to translate to the clinic.”
The study was published in eBioMedicine (The Lancet).
Related topics
Immunotherapy, near-infrared photoimmunotherapy (NIR-PIT), near-infrared photoimmunotherapy (NIR-PIT), Technology
Related conditions
Cancer
Related organisations
Nagoya University
Related people
Dr Kazuhide Sato