Improving ovarian cancer outcomes with artificial intelligence
Posted: 13 November 2023 | Drug Target Review | No comments yet
Researchers have developed an AI based model that is 80 percent accurate in predicting the therapy outcome of high-grade ovarian cancer.
An artificial intelligence (AI) based model called Integrated Radiogenomics for Ovarian Neoadjuvant therapy (IRON) has been developed to predict the therapy outcome, measured by volumetric reduction of tumour lesions, in 80 percent of high-grade ovarian cancer patients.
The technology is significantly better than current clinical methods with an accuracy of 80 percent. It analyses various patient clinical features, from circulating tumour DNA in the blood (liquid biopsy) to general characteristics such as age and health status, tumour markers, and disease images obtained through CT scans. This analysis provides a prediction of the therapy’s likelihood of success.
The AI model was developed by Dr Evis Sala’s team at the University of Cambridge and the study was organised by Dr Evis Sala, Chair of Diagnostic Imaging and Radiotherapy at the Faculty of Medicine and Surgery of the Catholic University and Director of the Advanced Radiology Center at the Policlinico Universitario A. Gemelli IRCCS.
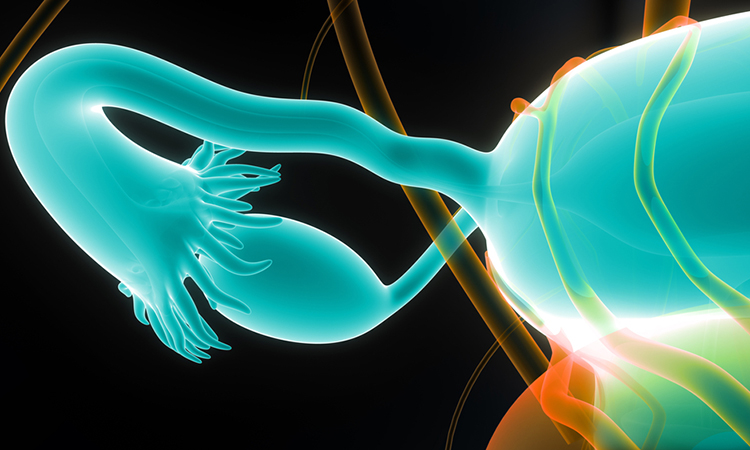
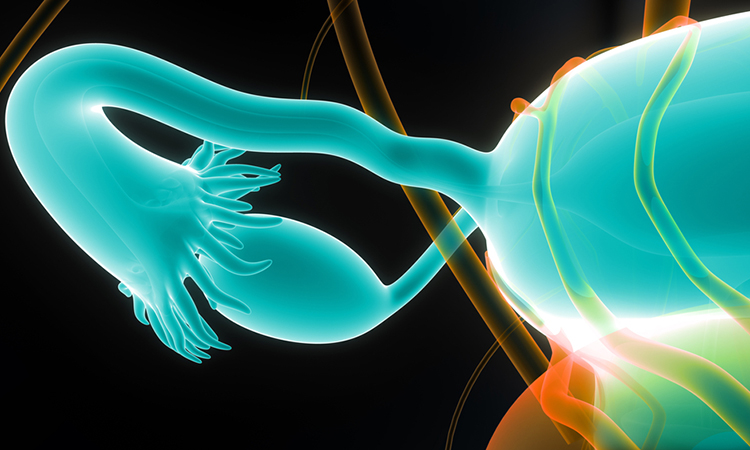
Ovarian cancer
Over 5,000 women in Italy are affected by ovarian cancer per year, which adds to the 30,000 patients who have already received a diagnosis. Diagnosis frequently occurs in advanced stages of disease as there is a lack of specific early symptoms. High-grade serous ovarian carcinoma, constituting 70 to 80 percent of ovarian tumours, is particularly aggressive and often resistant to chemotherapy. Therapy response prediction for this tumour type currently is only 50 percent accurate.
Furthermore, there are few clinically useful biomarkers for this cancer type because of its high heterogeneity which varies significantly from patient to patient. This highlighted the need for the development of an AI-based tool that was able to accurately predict chemotherapy responders.
Early identification
Dr Sala and Dr Mireia Crispin Ortuzar from the University of Cambridge explained: “We compiled two independent datasets with a total of 134 patients (92 cases in the first dataset, 42 in the second independent test set).” Clinicians collected data, including demographic information and treatment details, as well as blood biomarkers like CA-125 and circulating tumour DNA (ctDNA) from every patient. The CT scan images provided quantitative characteristics of all primary and metastatic tumour sites.
Initially, most of the disease burden was represented by omental and pelvic locations, common for ovarian cancer spread. In comparison to pelvic disease, omental deposits showed a better response to neoadjuvant therapy. Tumour mutations like the TP53 MAF assessed on circulating DNA and the marker CA-125 were correlated with overall disease burden before treatment and therapy response.
Also, the advanced analysis of CT scan images showed six patient subgroups with distinct biological and clinical characteristics, indicative of therapy response. The input data for the AI algorithms was all these tumour features. The developed model was then trained, and its effectiveness validated on an independent patient sample.
Future research
Dr Sala said: “From a clinical perspective, the proposed framework addresses the unmet need to early identify patients unlikely to respond to neoadjuvant therapy and may be directed to immediate surgical intervention.” She continued: “The tool could be applied to stratify the risk of each individual patient in future clinical research conducted at Policlinico Gemelli in collaboration with Professor Giovanni Scambia’s team, Chair of Gynaecology and Obstetrics at the Faculty of Medicine and Surgery of the Catholic University and Scientific Director of the Policlinico Universitario Agostino Gemelli IRCCS Foundation.”
This study was published in Nature Communications.
Related topics
Artificial Intelligence, Cancer research, DNA, Therapeutics
Related conditions
High-grade serous ovarian cancer (HGSOC)








