Delivering a human monoclonal IgG1 antibody to the brain
Posted: 5 January 2024 | Drug Target Review | No comments yet
Adding a biodegradable polymer at the hinge and near hinge regions of trastuzumab enabled its movement across the blood-brain barrier.
A new study by researchers at the University of Alabama at Birmingham reports that the site-directed addition of an FDA-approved, biodegradable polymer at the hinge and near hinge regions of the therapeutic antibody trastuzumab effectively facilitated the brain delivery of a human monoclonal IgG1 antibody.
The blood-brain barrier (BBB) prevents antibodies entering the brain, which limits the potential use of antibody therapeutics to treat brain diseases. Over 100 United States Food and Drug Administration (FDA)-approved therapeutic antibodies are used to treat cancers and autoimmune, infectious, and metabolic diseases. Discovering methods to transport therapeutic antibodies across the BBB from the peripheral blood stream into the central nervous system could create useful treatments that act in the brain.
The first work on this new platform included in vitro and mouse-model experiments. Although the team said the delivery system needs to be optimised and tested further, they noted their simple methodology converts antibody therapeutics to a brain-deliverable form that maintains the antibody’s medical functionality.
Dr Masakazu Kamata, leader of the study and an associate professor in the UAB Department of Microbiology, explained: “In this context, this simple methodology has great potential to serve as the platform to not only repurpose the current antibody therapeutics, but also encourage the design of novel antibodies, for the treatment of brain diseases.”
Modifying antibodies
Poly 2-methacryloyloxyethyl phosphorylcholine (PMPC), with chain lengths of 50, 100 or 200 monomers, was the biocompatible polymer used. The team had already discovered that this non-immunogenic polymer, which the FDA has approved as a coating material for transplantable devices, could bind to two receptors on brain microvascular endothelial cells composing the BBB.
Those cells could then move the polymer across the BBB by transcytosis, a specialised transport whereby extracellular cargo is brought inside the cell, shuttled across the cytoplasm to the other side of the cell, and then released.
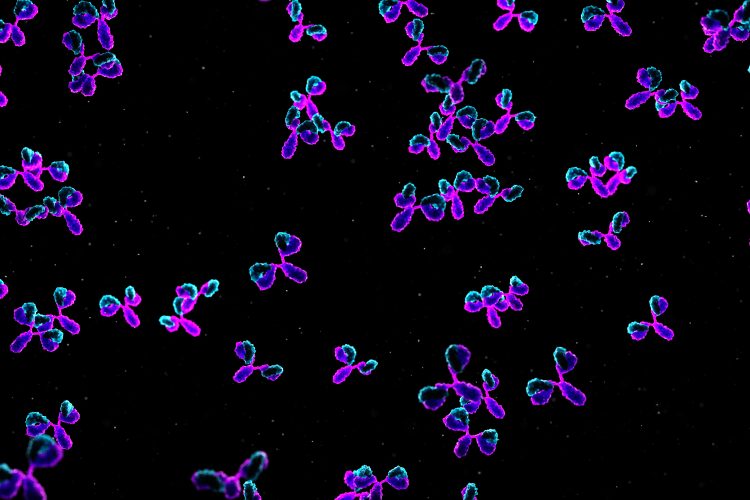
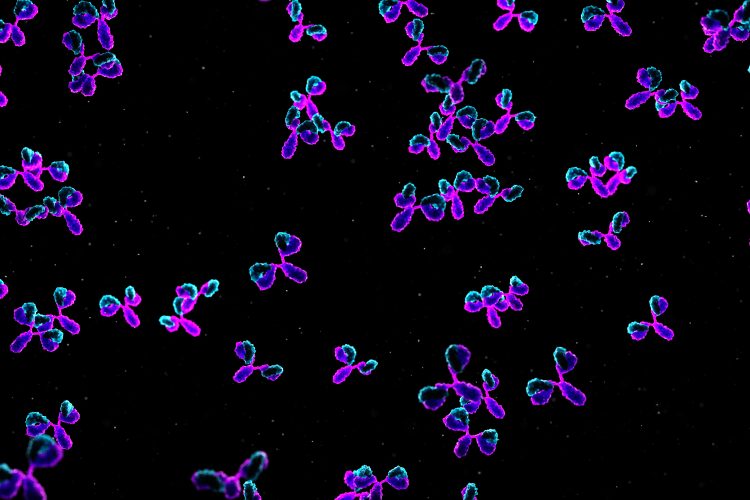
The researchers cleaved four interchain disulfide bonds in the trastuzumab IgG1 hinge and near hinge regions, creating thiol groups. Each thiol group was conjugated to a chain of the PMPC to form trastuzumab molecules with one of the three chain lengths, which they denoted as Tmab-PMPC50, Tmab-PMPC100 and Tmab-PMPC200.
Each of these modified antibodies maintained trastuzumab-specific binding to cells expressing the HER2 antigen, the target of trastuzumab. Both the Tmab-PMPC50 and the Tmab-PMPC100 were internalised into HER2-positive cells and promoted antibody-dependent cell death, which is the medical functionality by which trastuzumab kills HER2+ breast cancer cells.
“Those findings collectively indicate that PMPC conjugation achieves effective brain delivery of therapeutic antibodies, such as trastuzumab, without induction of adverse effects, at least in the liver, the blood-brain barrier or the brain,”
Then, the scientists demonstrated that PMPC conjugation of trastuzumab enhanced BBB penetration through the epithelial cells on the BBB via the transcytosis pathway. The translocatable Tmab-PMPC100 was the best at efficient BBB penetration while retaining trastuzumab’s epitope recognition, the ability of the antibody to bind to its antigen target.
Both Tmab-PMPC100 and Tmab-PMPC200 were about fivefold better at brain penetration than native trastuzumab in a mouse model. In preliminary in vitro and mouse-model experiments, the polymer-modified trastuzumab did not induce neurotoxicity, show adverse effects in the liver, or disrupt the integrity of the BBB.
“Those findings collectively indicate that PMPC conjugation achieves effective brain delivery of therapeutic antibodies, such as trastuzumab, without induction of adverse effects, at least in the liver, the blood-brain barrier or the brain,” Kamata said.
The team noted that others have also investigated methods to get antibodies across the BBB. In the work leading up to the new study, the team had shown they could wrap numerous macromolecular cargos within PMPC shells. These nanocapsules demonstrated prolonged blood circulation, reduced immunogenicity and enhanced brain delivery in mice and non-human primates.
However, nanocapsules required the addition of targeting ligands to bring them to their disease target and degradable crosslinkers that would allow release of the cargo at that site. Disease-associated microenvironments often lack conditions that can trigger degradation of the crosslinkers.
PMPC does not exhibit undesirable traits that other various ligands to boost transport do. Ligands derived from microbes and toxins, or endogenous proteins like lipoproteins, have been studied by other researchers, but they typically have undesirable surface properties, such as being highly immunogenic, highly hydrophobic or charged.
This study was published in Frontiers in Cell and Developmental Biology.
Related topics
Antibodies, Drug Targets, In Vitro, Ligands, Polymers
Related conditions
autoimmune diseases, Cancer, Infectious diseases, metabolic disease
Related organisations
Food and Drug Administration (FDA), University of Alabama at Birmingham (UAB)
Related people
Dr Masakazu Kamata (UAB)








