Melanoma tumours produce altBRAFs by genomic deletions
Posted: 15 April 2024 | Drug Target Review | No comments yet
The discovery that genomic deletions cause altBRAFs can help develop new therapies to overcome drug resistance in BRAF-mutant melanoma.
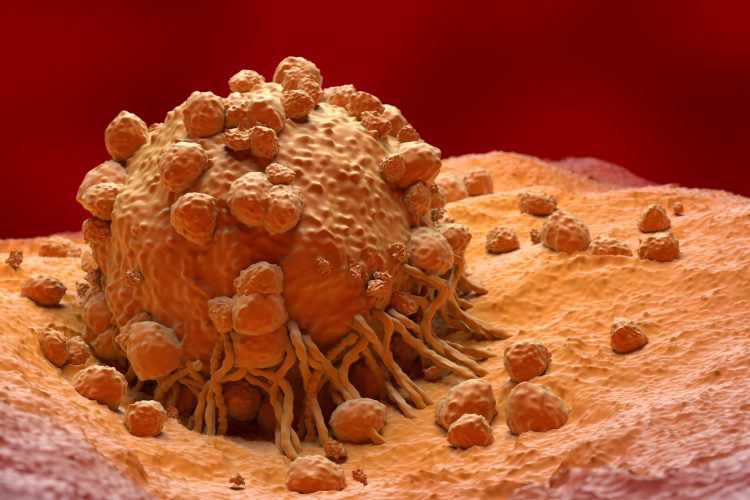
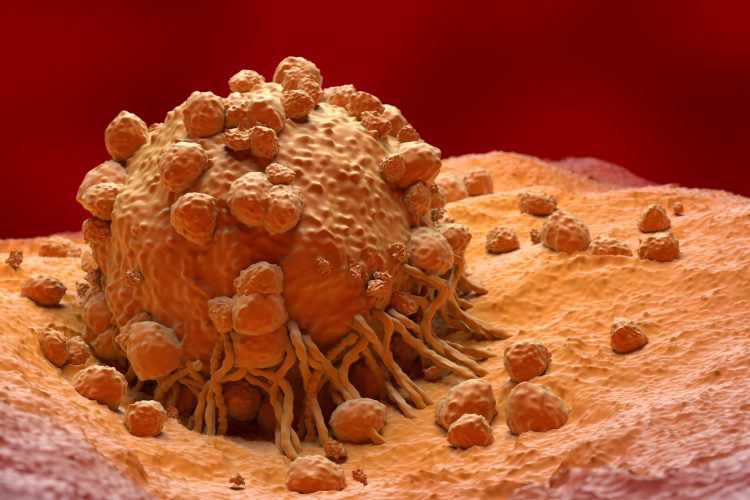
Researchers at the Centre for Genomic Regulation (CRG) have discovered one of the mechanisms through which melanoma drug resistance occurs. Global incidences of the deadliest form of skin cancer are rising, meaning that more effective treatments are required.
About one in two melanoma patients will have mutations in the BRAF gene which cause the cells to divide uncontrollably. The discovery of BRAF mutations has led to development of targeted therapies to inhibit its function. In the last decade, a standard treatment option for melanoma has been to simultaneously target both BRAF mutations and MEK, two genes that are part of the MAPK signalling pathway. In cancer, this pathway is rewired for uncontrolled growth, so targeting two different critical points slows or stops cancer growth.
However, although the combined use of first-generation inhibitors prompt good initial responses, around 50 percent of melanoma patients with BRAF mutations will relapse within one year. Other mechanisms, which remain poorly understood, reactivate the MAPK pathway and cause this drug resistance. Dr Francisco Aya Moreno, oncologist and recent PhD graduate at the CRG, explained: “Melanoma drug resistance is a huge clinical problem because it occurs in almost all BRAF-mutated patients under BRAF/MEK inhibitor therapy and there are few or no therapeutic alternatives. There is an urgent need to understand the many different underlying mechanisms and find new strategies to deal with this constantly evolving arms race.”
The new study found in various lab models and patient tumour samples that melanoma tumours produce alternative versions of the BRAF protein (altBRAFs) by genomic deletions. The altBRAFs lack regions targeted by BRAF inhibitors, reactivating the MAPK pathway and making the drugs less effective. Previously, altBRAFs were thought to be made through alternative splicing, but the discovery that genomic deletions are instead the cause means researchers must shift away from proposals for using drugs that target splicing as a therapeutic strategy.
Co-author of the study Dr Juan Valcarcel, researcher at the CRG and ICREA Research Professor commented: “For years, we’ve known that some patients produce altBRAFs and these help the cancer resist treatment, but we misunderstood the mechanism behind their creation. Knowing that genomic deletions are the cause opens new avenues for developing therapies that could more effectively help patients with BRAF mutations.”
Notably, the scientists found evidence of the same genomic deletions in melanomas which had not been treated yet, indicating that melanomas can naturally develop mechanisms that mimic drug resistance, even without exposure to drugs. Genetic testing in a clinical setting before treatment begins could identify and target these early resistance mechanisms and therefore improve the efficacy of first-line therapies.
Moreover, further analyses showed that genomic deletions could be a more widespread mechanism of oncogenesis and resistance than previously thought. Although rare, researchers found evidence of altBRAFs in melanomas with a normal-functioning BRAF gene, as well as in other types of cancers, including breast, kidney, prostate and non-small cell lung cancer (NSCLC).
“There is an emerging class of drugs known as second generation RAF inhibitors. Unlike BRAF inhibitors, these drugs have a broad spectrum, and so could potentially inhibit the function of altBRAFs. Clinical trials which are assessing their effectiveness should also expand to include melanoma patients with a normal functioning BRAF gene as well, and possibly to other cancer types which express altBRAFs,” added Dr Aya Moreno.
This study was published in Cell Reports.
Related topics
Cancer research, Drug Targets, Genetic Analysis, Genomics, Oncology, Therapeutics
Related conditions
Cancer Research, Melanoma
Related organisations
Centre for Genomic Regulation (CGR)
Related people
Dr Francisco Aya Moreno (CRG), Dr Juan Valcarcel (CRG)








