Accelerating cardiac regenerative therapy with HiPSC spheroids
Posted: 29 April 2024 | Drug Target Review | No comments yet
Injections of cardiac spheroids into primate ventricles improved left ventricular ejection after four weeks.

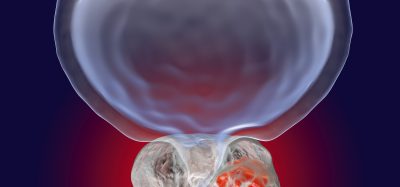
Researchers from Shinshu University and Keio University School of Medicine have tested a novel strategy for regenerative heart therapy. They transplanted cardiac spheroids derived from human induced pluripotent stem cells (HiPSCs) into damaged ventricles and observed very positive outcomes in primate models. These results could expand treatment options for people suffering from heart problems.
The prevalence of myocardial infarction is rising. These destroy millions of cardiac muscle cells, leaving the heart in a weakened state. Currently, as mammals cannot regenerate cardiac muscle cells on their own, heart transplants are the only clinically viable option for patients suffering heart failure. However, full heart transplants are expensive and donors are rare, so alternative therapies are highly sought after.
The team cultivated HiPSCs in a medium that led to their differentiation into cardiomyocytes. Following the extraction and purification of cardiac spheroids, they injected approximately 6 × 107 cells into the damaged hearts of crab-eating macaques and monitored the condition of the animals for twelve weeks, taking regular measurements of cardiac function.
Analysis of the monkeys’ hearts at the tissue level was then conducted to assess whether cardiac spheroids could regenerate the damaged heart muscles. The researchers verified the correct reprogramming of HiPSCs into cardiomyocytes first, observing at cellular-level electrical measurements that the cultured cells showed patterns typical of ventricular cells. Also, the cells responded as expected to numerous known drugs. Significantly, they discovered that the cells abundantly expressed adhesive proteins like connexin 43 and N-cadherin, which would promote their vascular integration into an existing heart.
Furthermore, this approach is less expensive and easier to adopt because the cells were transported from the production facility at Keio University to Shinshu University, located 230km away. The cardiac spheroids were preserved at 4°C in standard containers and withstood the four-hour journey, meaning extreme cryogenic measures would not be required when transporting the cells to clinics.
The monkeys received injections of either cardiac spheroids or a placebo directly into the damaged heart ventricle. The team noted that arrhythmias were very uncommon, with only two individuals experiencing transient tachycardia in the first two weeks among the treatment group. Echocardiography and computed tomography exams confirmed that, compared to the control group, the hearts of monkeys that received treatment had better left ventricular ejection after four weeks, demonstrating a superior blood pumping capability.
Ultimately, it was revealed through the histological analysis that the cardiac grafts were mature and properly connected to pre-existing existing tissue, confirming the results of previous observations. “HiPSC-derived cardiac spheroids could potentially serve as an optimal form of cardiomyocyte products for heart regeneration, given their straightforward generation process and effectiveness,” explained first author Dr Hideki Kobayashi. “We believe that the results of this research will help solve the major issue of ventricular arrhythmia that occurs after cell transplantation and will greatly accelerate the realisation of cardiac regenerative therapy.”
Despite this cardiac spheroid production protocol being tested in monkeys, it was designed for clinical application in humans. “The favourable results obtained thus far are sufficient to provide a green light for our clinical trial, called the LAPiS trial. We are already employing the same cardiac spheroids on patients with ischemic cardiomyopathy,” concluded Dr Kobayashi.
This study was published in Circulation.
Related topics
Induced Pluripotent Stem Cells (iPSCs), Regenerative Medicine, Spheroids, Stem Cells, Therapeutics
Related conditions
cardiovascular diseases, myocardial infarction, Ventricular arrhythmias
Related organisations
Keio University School of Medicine, Shinshu University
Related people
Dr Hideki Kobayashi (Shinshu University)